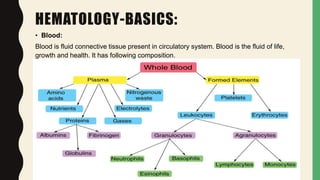
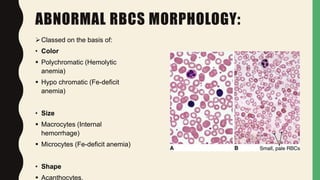
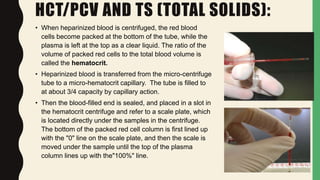
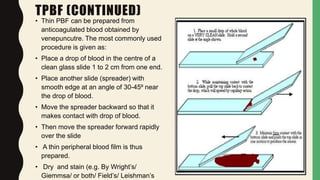
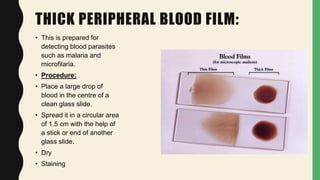
The document outlines the importance of hematological examination in veterinary medicine, detailing various tests such as complete blood count (CBC) and blood smears for diagnosing conditions. It discusses the significance of evaluating erythrocytes and leukocytes, the methodology involved in manual counts, and the interpretation of results related to diseases. Additionally, it covers modern technology like the XP-300 hematology analyzer and reviews common blood disorders and their implications.