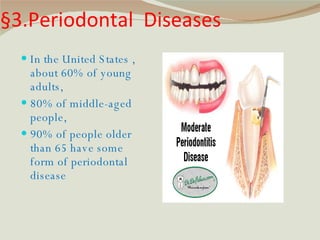
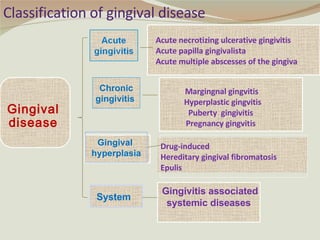
Periodontal diseases affect the tissues around the teeth and range from gingivitis to periodontitis. About 60-90% of people have some form of periodontal disease depending on age. Periodontal diseases are caused by bacterial dental plaque which leads to inflammation if not removed regularly. The bacteria can damage gum tissue, bone, and ligaments supporting the teeth. Periodontal diseases are classified based on severity from gingivitis to chronic periodontitis with bone loss. Treatment focuses on improving oral hygiene through regular cleaning to control the bacterial plaque.