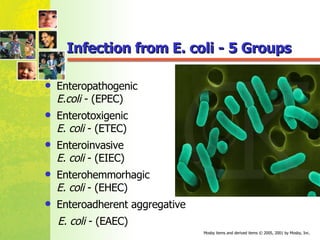
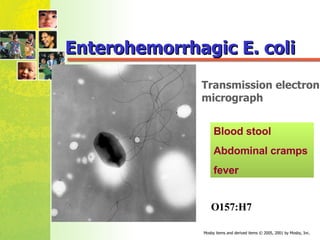
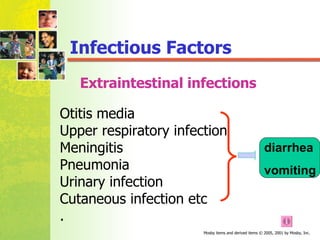
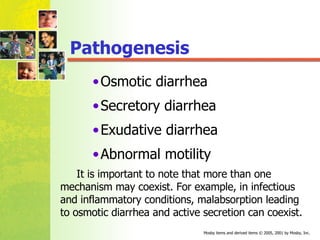
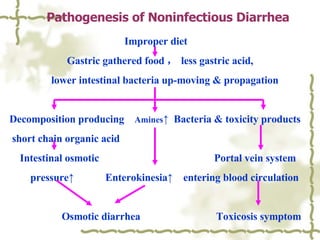
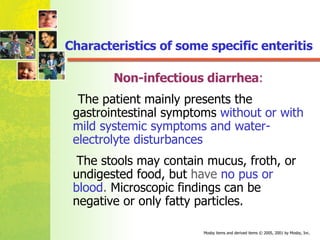
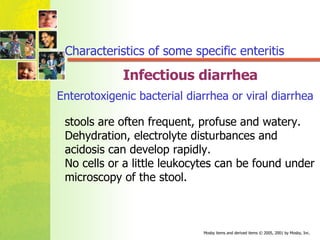
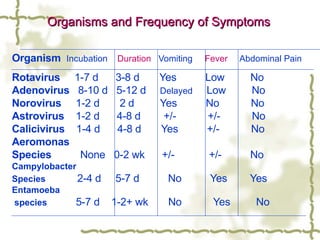
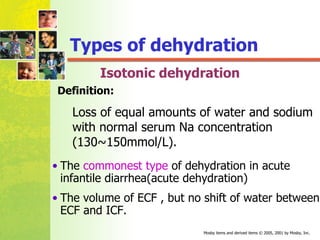
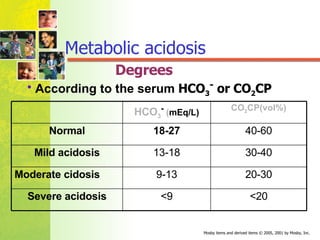
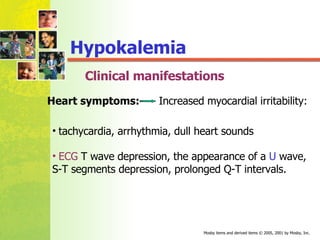
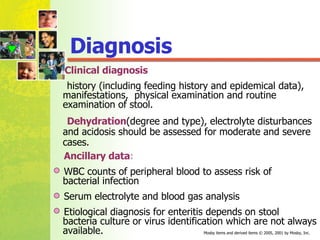
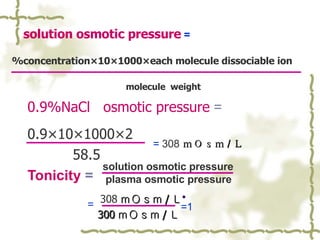
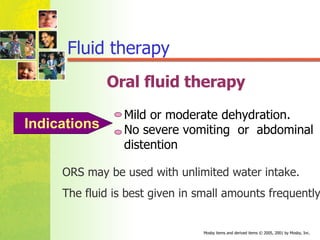
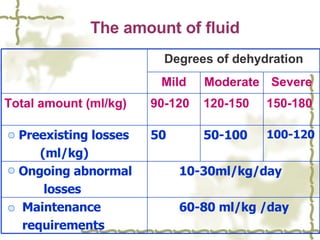
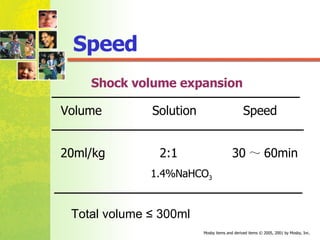
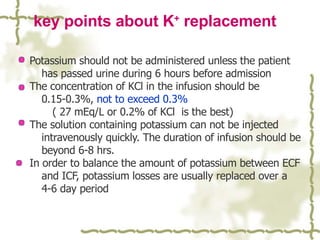
The document discusses infantile diarrhea including its etiology, pathogenesis, clinical manifestations, diagnosis, and treatment. It causes are multi-factorial and can be infectious, like rotavirus or E. coli, or non-infectious, like improper diet. Pathogenesis involves mechanisms like osmotic diarrhea, secretory diarrhea, or abnormal motility. Clinical manifestations include gastrointestinal symptoms, systemic toxic symptoms, and water/electrolyte disturbances. Diagnosis is based on symptoms and stool examination. Treatment focuses on rehydration and correcting water/electrolyte imbalances.