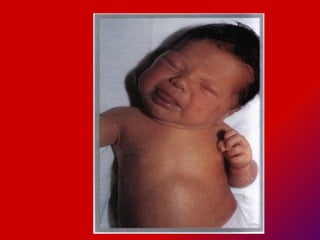
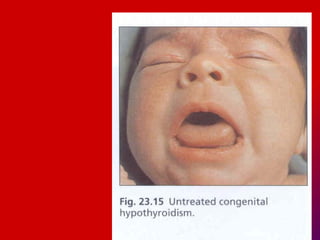
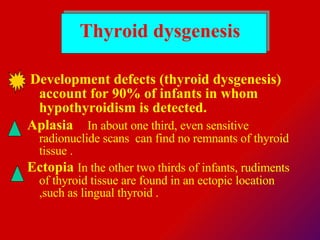
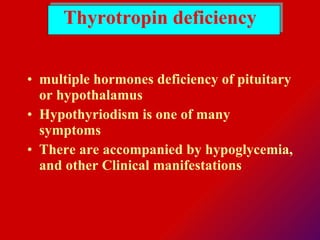
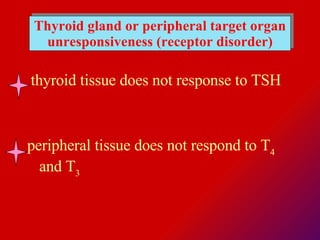
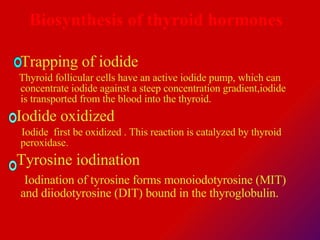
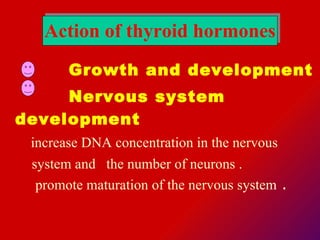
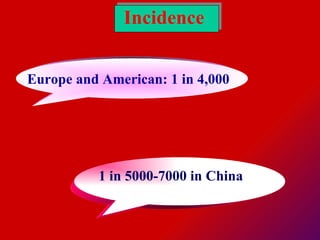
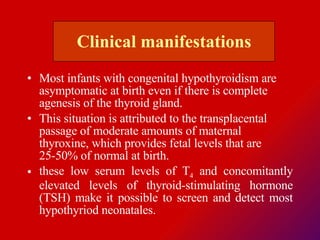
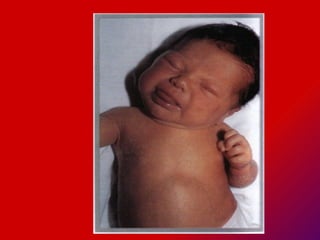
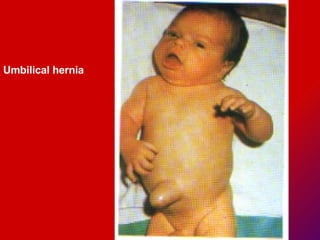
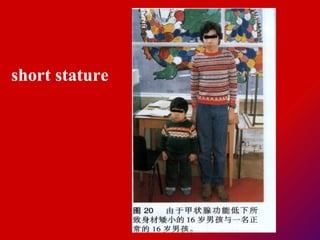
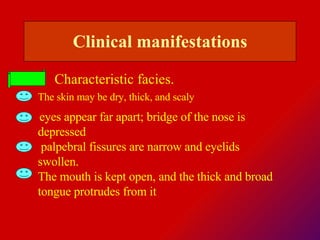
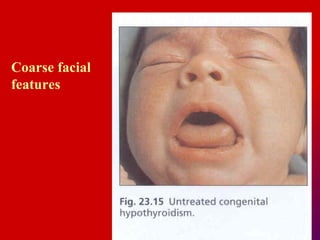
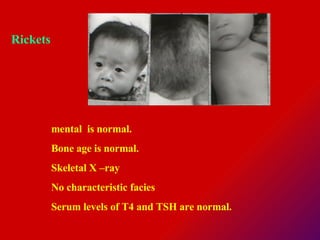
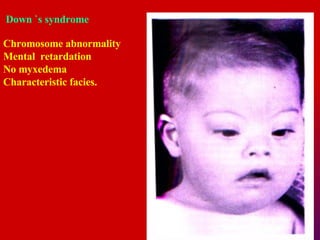
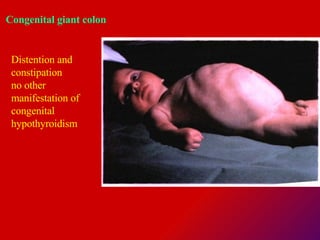
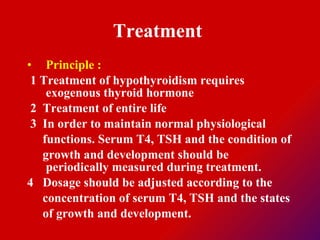
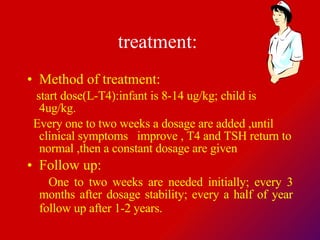
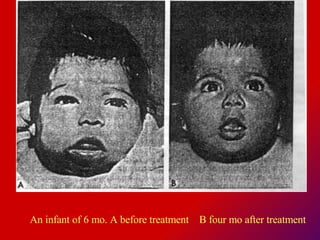
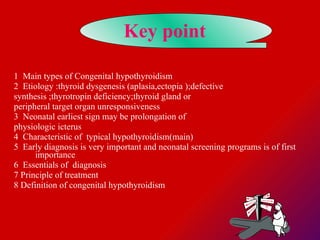
Congenital hypothyroidism results from deficient thyroid hormone production or receptor defects. It can cause growth retardation and impaired mental development if not treated. The document discusses the types, causes, signs, diagnosis, and lifelong treatment of the disorder, which involves replacing thyroid hormone to maintain normal physiology and development. Early diagnosis and treatment through newborn screening programs can prevent intellectual disability and allow normal growth.