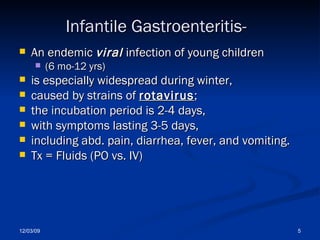
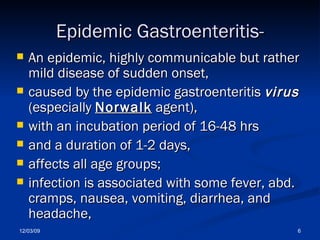
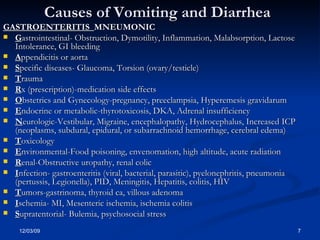
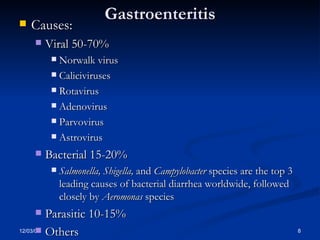
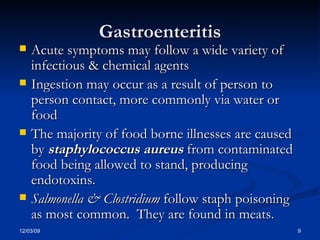
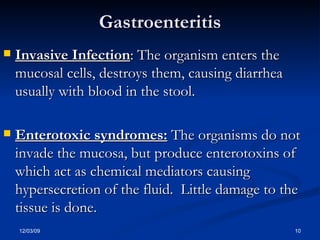
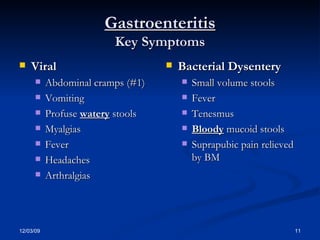
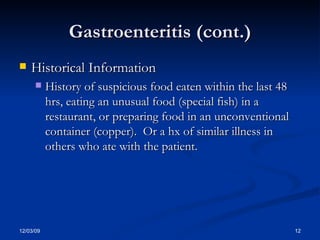
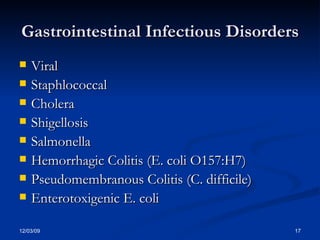
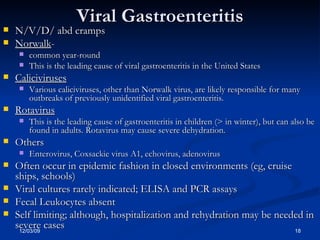
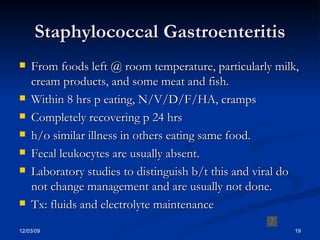
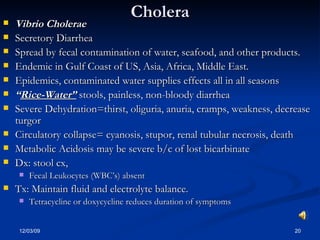
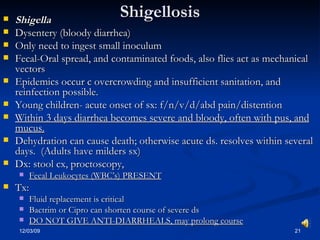
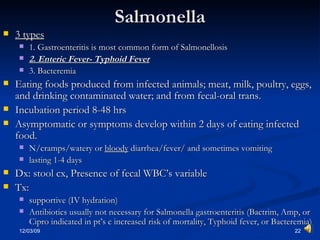
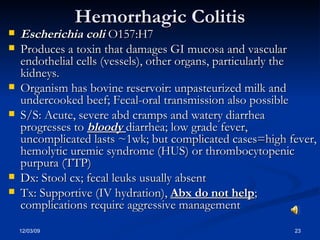
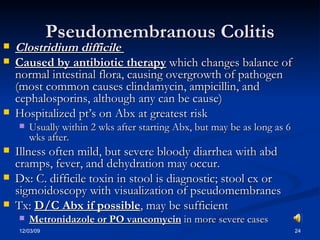
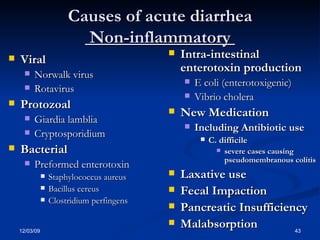
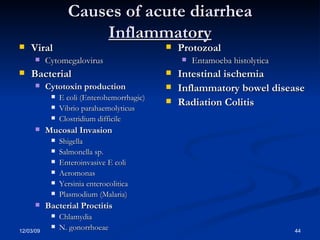
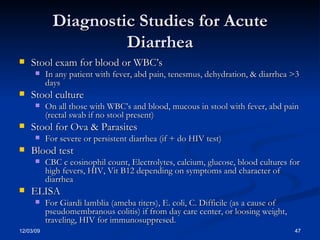
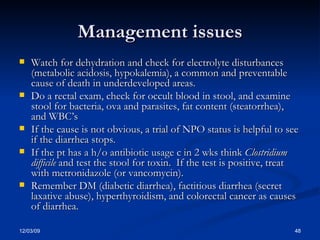
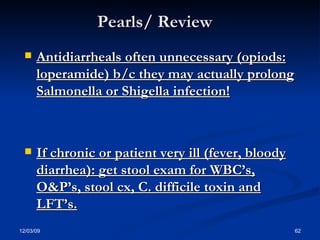
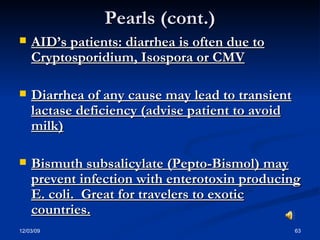
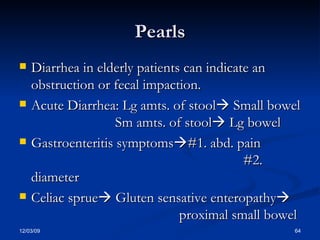
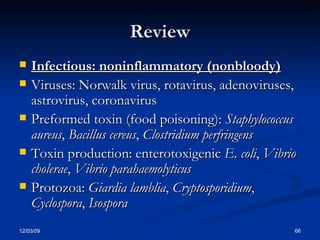
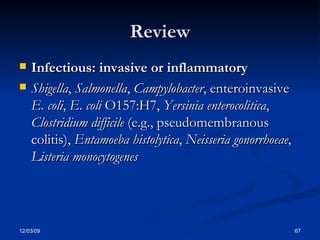
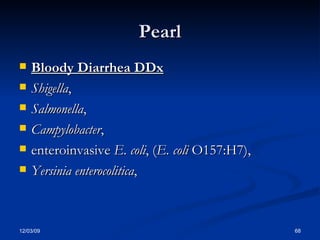
Gastroenteritis refers to inflammation of the stomach and intestines that commonly causes diarrhea, nausea, and vomiting. It is usually caused by infectious agents like viruses, bacteria, or parasites that damage the intestinal lining. The main goals of treatment are rehydration and electrolyte replacement to prevent dehydration. Specific infectious causes discussed in the document include norovirus, rotavirus, salmonella, shigella, E. coli O157:H7, and Clostridium difficile.