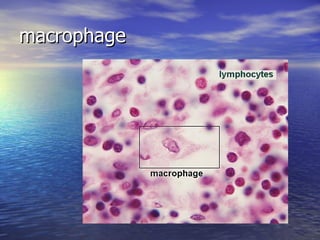
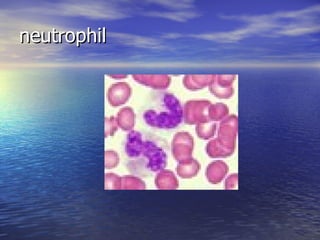
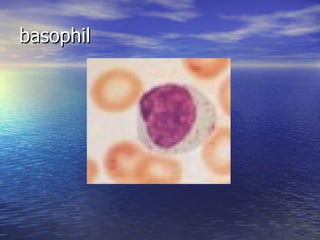
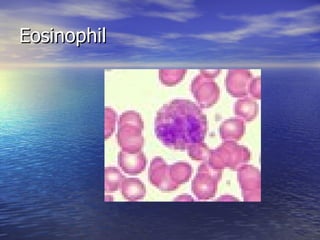
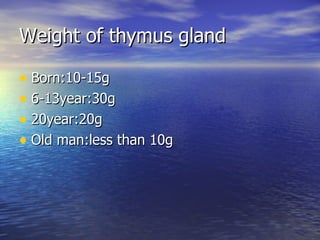
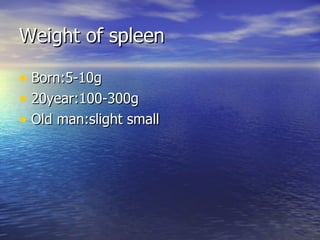
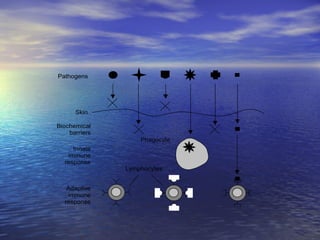
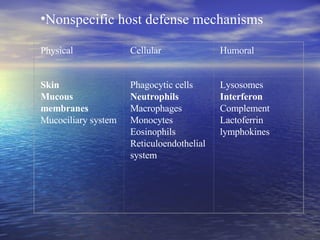
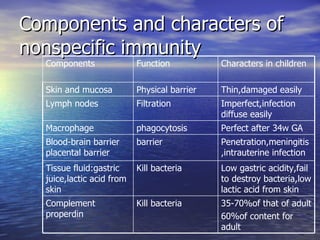
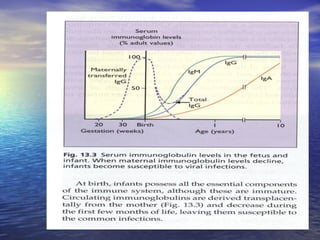
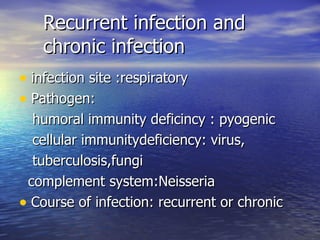
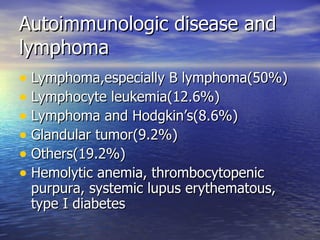
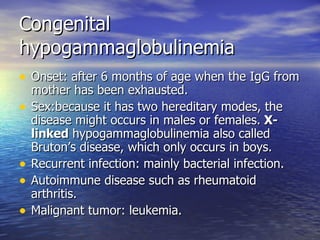
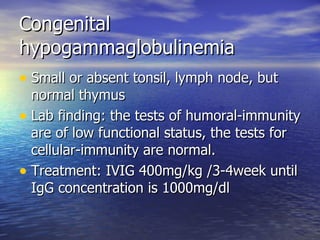
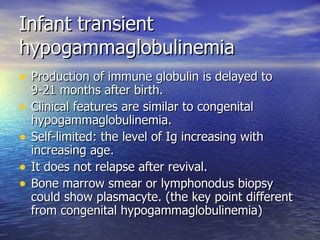
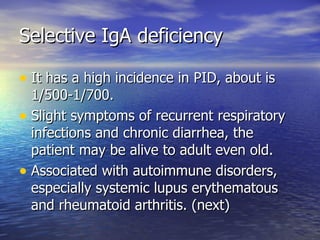
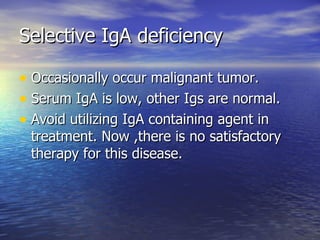
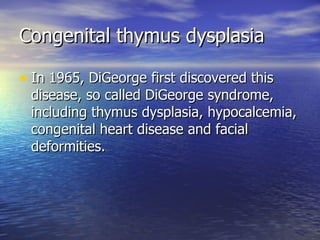
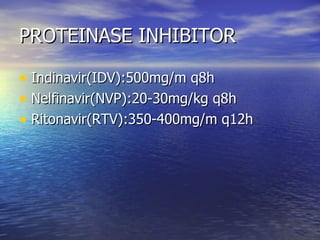
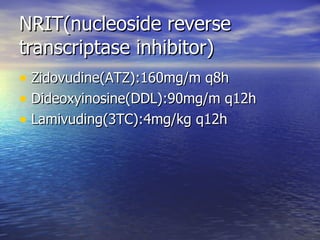
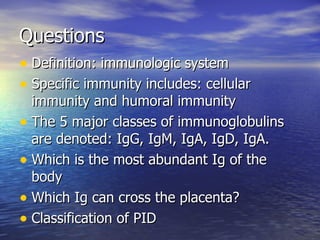
The document summarizes characteristics of the immunologic system and immunodeficiency diseases. It describes the components and functions of nonspecific and specific immunity. It discusses the development of T cells and B cells and the five classes of immunoglobulins. It also classifies primary immunodeficiency diseases and describes some common conditions in children like congenital hypogammaglobulinemia.
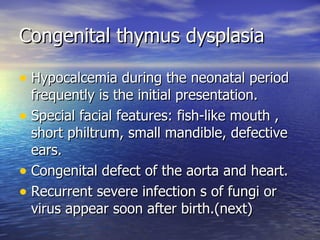
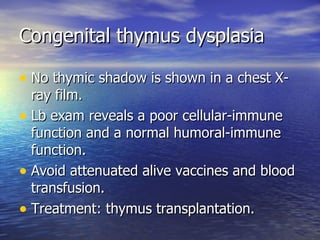
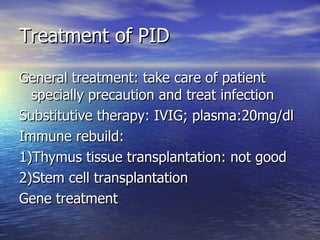
![Immunodeficiency diseases Classification Some common diseases due to immunodeficiency in children (congenital hypogammaglobulinemia, infant transient hypogammaglobulinemia, selective IgA deficiency, congenital thymus dysplasia [DiGeorge’s syndrome], AIDS)](https://image.slidesharecdn.com/chapter4immunologicsystem-090507064234-phpapp01/85/Chapter-4-Immunologic-System-4-320.jpg)