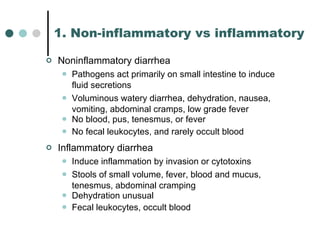
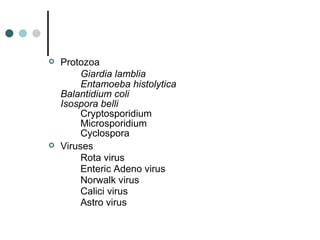
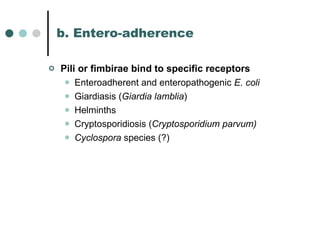
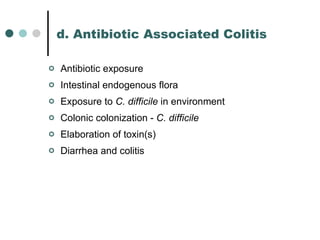
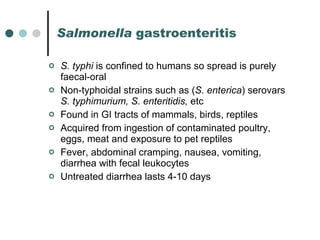
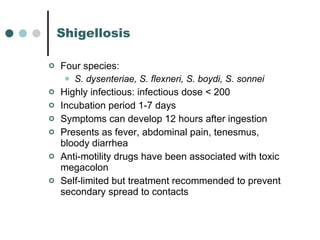
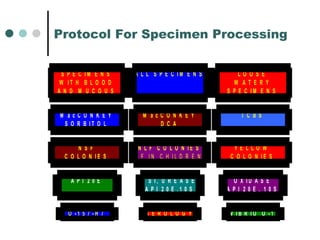
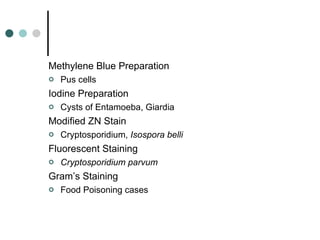
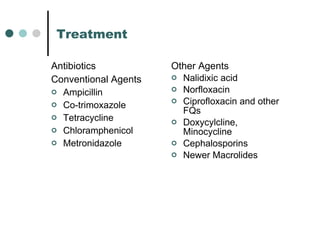
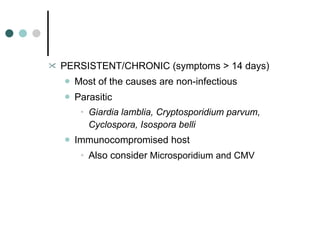
The document discusses various types of gastro-intestinal infections and diarrheas. It describes the classification, symptoms, pathogens, transmission, and treatments for infectious diarrheas including bacterial, protozoal and viral causes. Key causes discussed are Salmonella, Shigella, E.coli, Campylobacter, Giardia, Clostridium difficile and rotavirus. The pathophysiology and diagnostic approach are also summarized.
































![3. Low-versus high-volume diarrhea Low volume (low water): colonic High volume (high water): small bowel OSMOTIC DIARRHEA: high-volume diarrhea in which the measured fecal osmolality is less than 2 [Na + K] Sorbitol-containing liquid medications, tube feedings, lactose intolerance SECRETORY DIARRHEA: high-volume diarrhea in which the measured fecal osmolality equals 2 [Na + K] E. Coli , rotavirus, laxative abuse](https://image.slidesharecdn.com/giinfections-100624143703-phpapp02/85/Gi-infections-47-320.jpg)