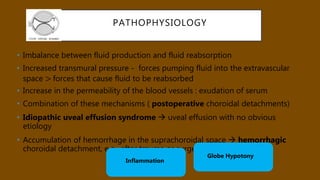
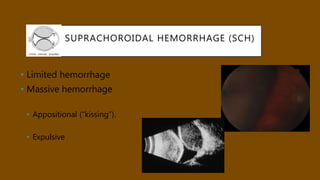
This document provides information on choroidal effusions and detachment. It defines choroidal effusions as the accumulation of fluid in the suprachoroidal space between the choroid and sclera. The document discusses the anatomy of the choroid, types of effusions (serous and hemorrhagic), causes including inflammation and changes in fluid balance, diagnosis using imaging like B-scan ultrasound, and management including observation, medications, and surgery. Risk factors, presentations, and differential diagnoses of different conditions that can cause choroidal effusions are also covered.