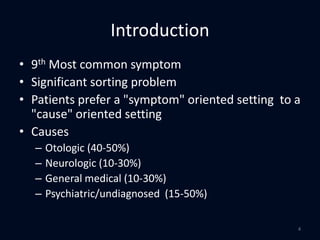
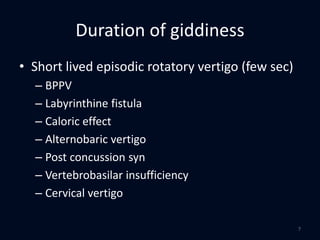
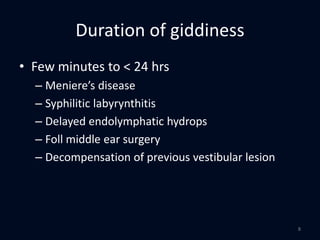
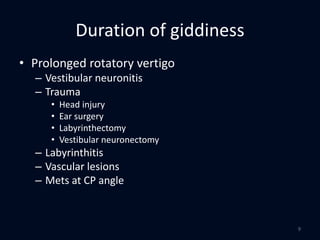
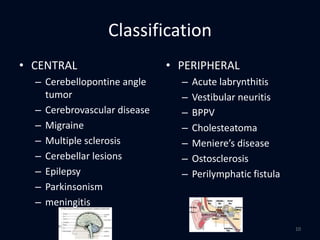
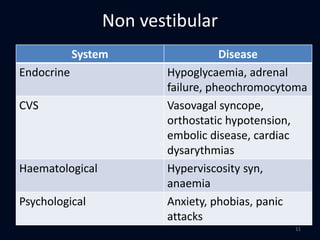
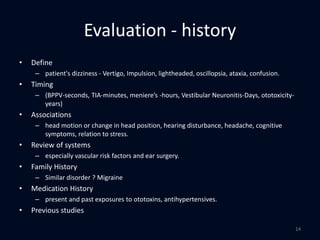
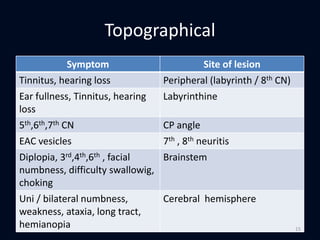
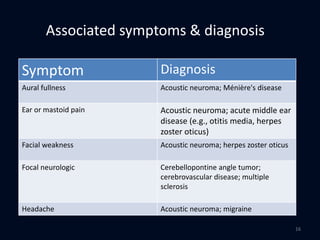
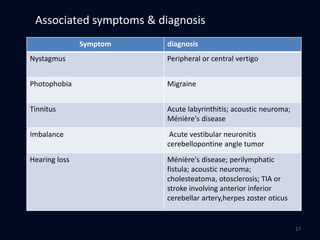
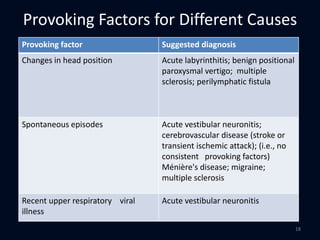
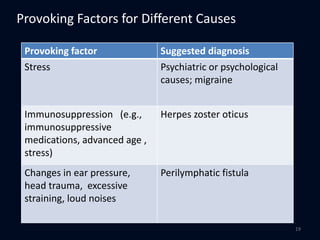
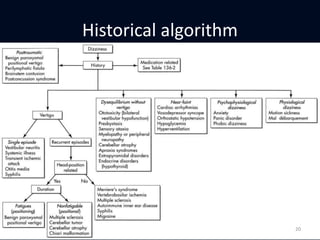
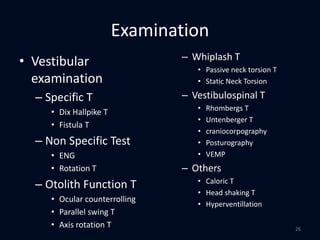
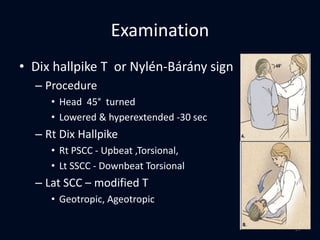
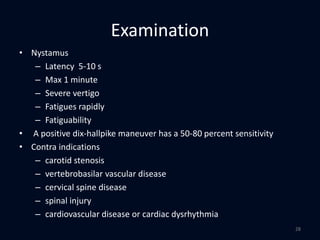
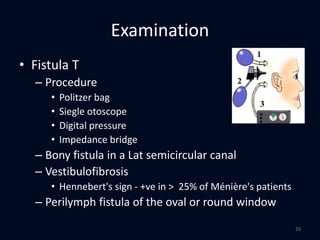
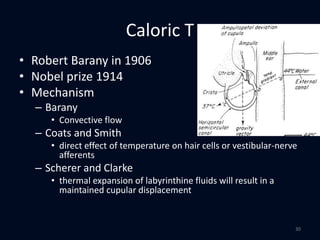
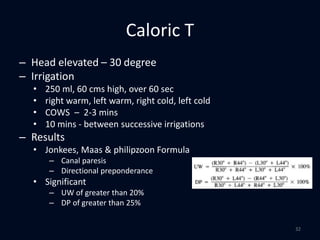
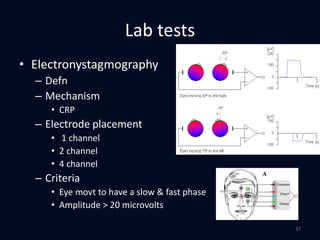
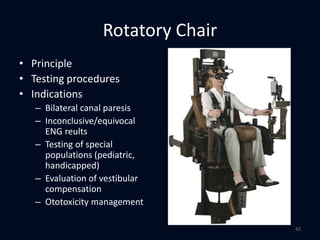
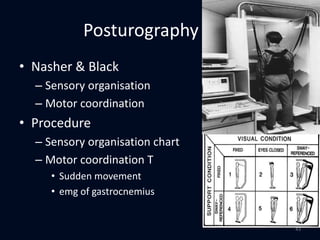
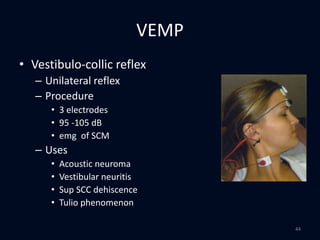
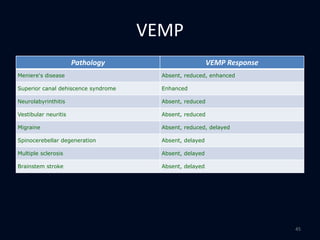
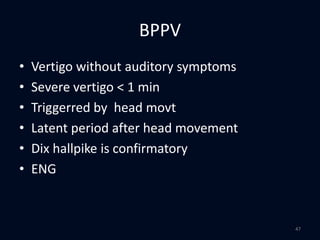
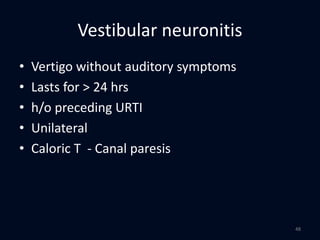
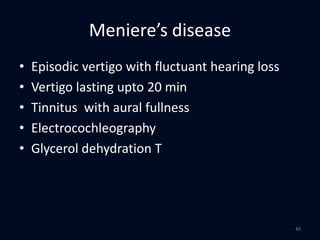
This document provides an overview of evaluating patients presenting with dizziness or vertigo. It discusses classifying vertigo based on duration, whether it is central or peripheral in origin, and non-vestibular causes. A thorough history and physical exam including neurologic and vestibular testing is outlined. Key diagnostic tests like Dix-Hallpike, caloric testing, and VEMP are described. Common causes of vertigo like BPPV, vestibular neuronitis, and Meniere's disease are highlighted based on presenting symptoms, exam findings, and test results.