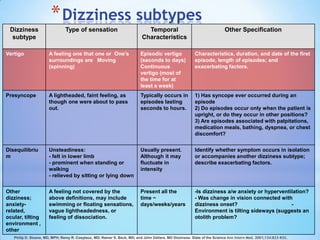
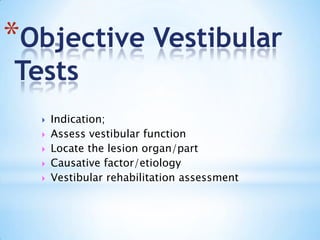
This document provides information on dizziness and balance disorders from Dr. Zuraida Zainun, a senior lecturer in audiology. It includes definitions of dizziness, descriptions of different dizziness subtypes, factors to consider in the history and examination of patients with dizziness, details on various vestibular and balance tests, differential diagnoses, and concepts of management including vestibular rehabilitation exercises and follow up. References are also provided on topics related to dizziness and balance disorders.