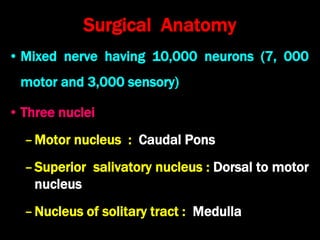
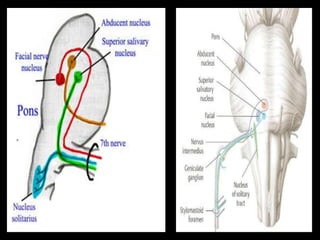
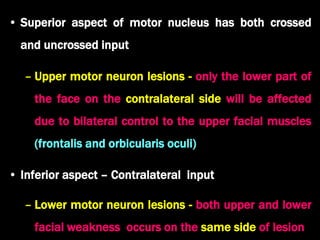
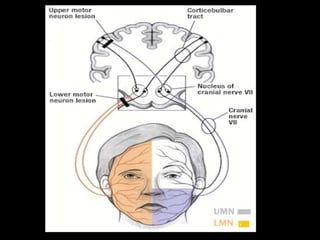
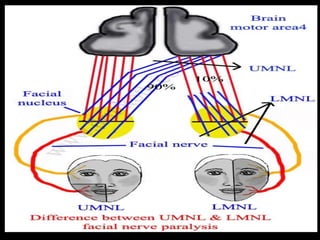
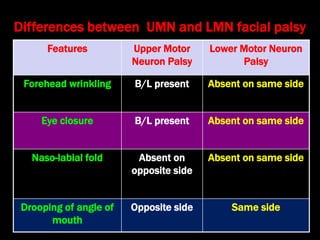
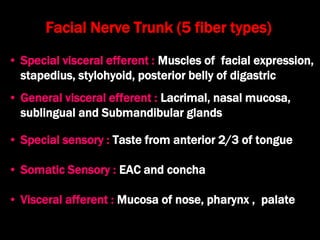
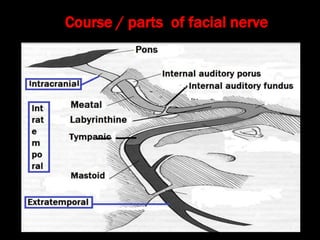
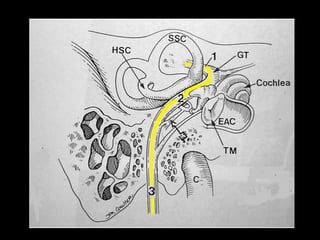
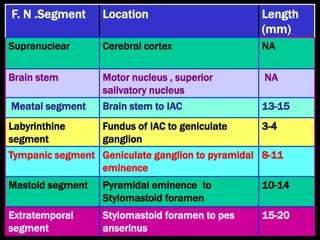
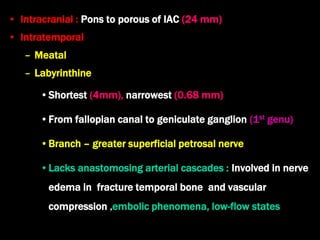
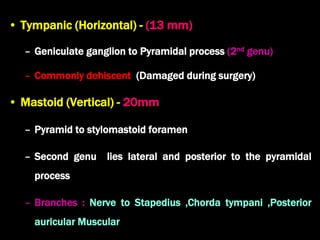
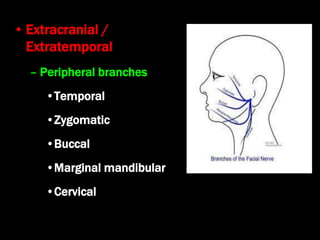
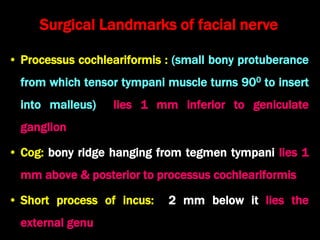
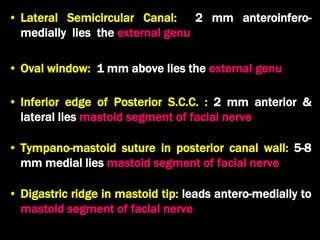
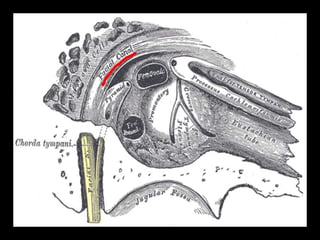
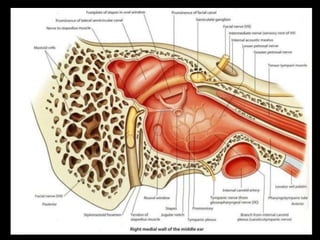
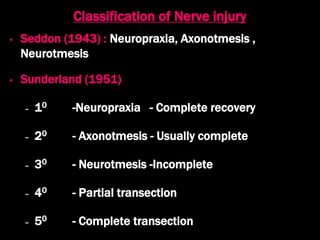
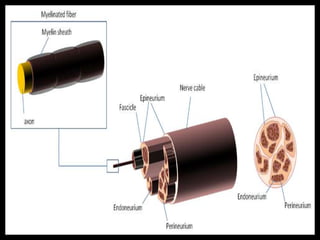
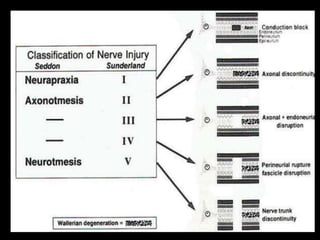
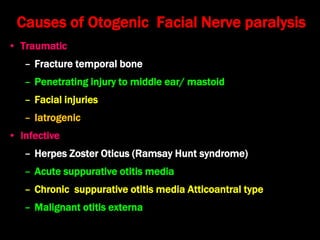
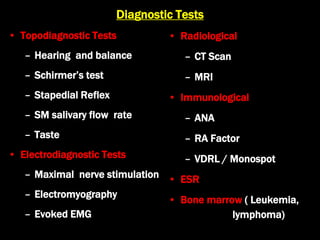
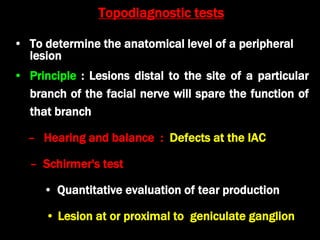
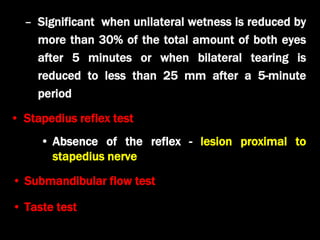
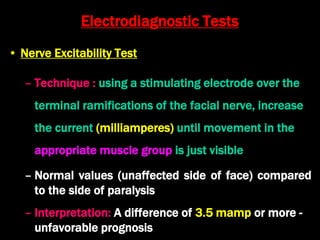
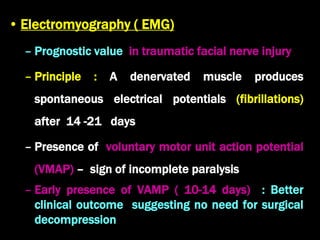
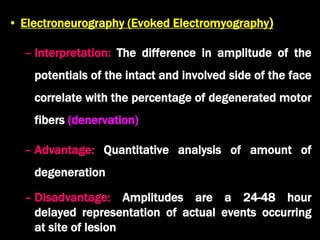
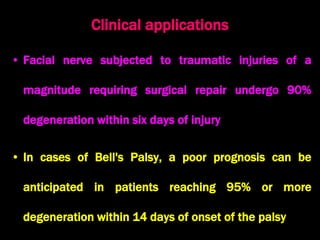
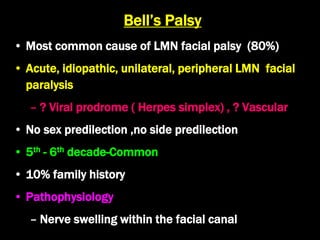
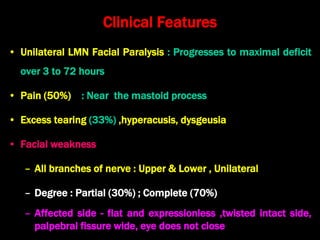
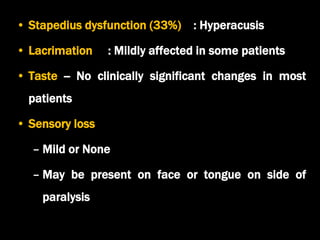
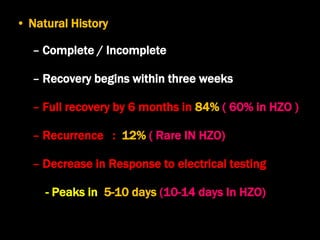
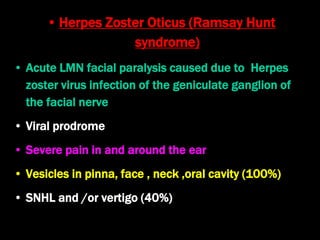
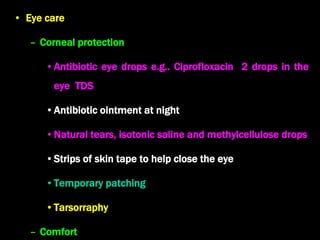
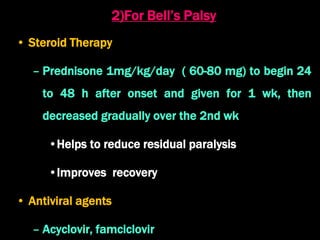
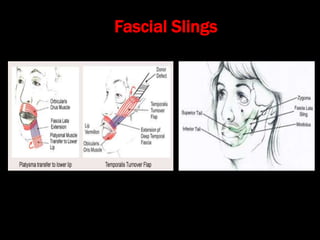
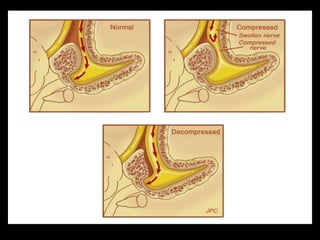
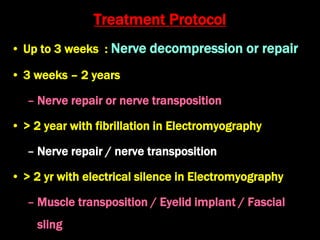
The document discusses disorders of the facial nerve, including their anatomy, causes, diagnostic tests, and treatment options. It highlights differences between upper and lower motor neuron lesions, common conditions like Bell's palsy and Ramsay Hunt syndrome, as well as recommendations for medical and surgical management of facial nerve paralysis. Additionally, it outlines the classification of nerve injuries and the prognosis related to various facial nerve disorders.