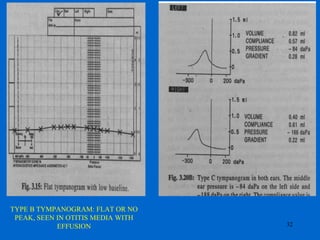
Otitis media with effusion, also known as serous otitis media or glue ear, is defined as the chronic accumulation of fluid in the middle ear caused by Eustachian tube dysfunction. It is a common reason for pediatric visits and the most frequent cause of hearing loss in children. Risk factors include young age, male gender, attendance at daycare, and winter season. Diagnosis involves tympanometry showing a flat tympanic membrane and treatment options include watchful waiting, antibiotics, myringotomy with tube insertion, or adenoidectomy. Complications can include permanent hearing loss if left untreated.