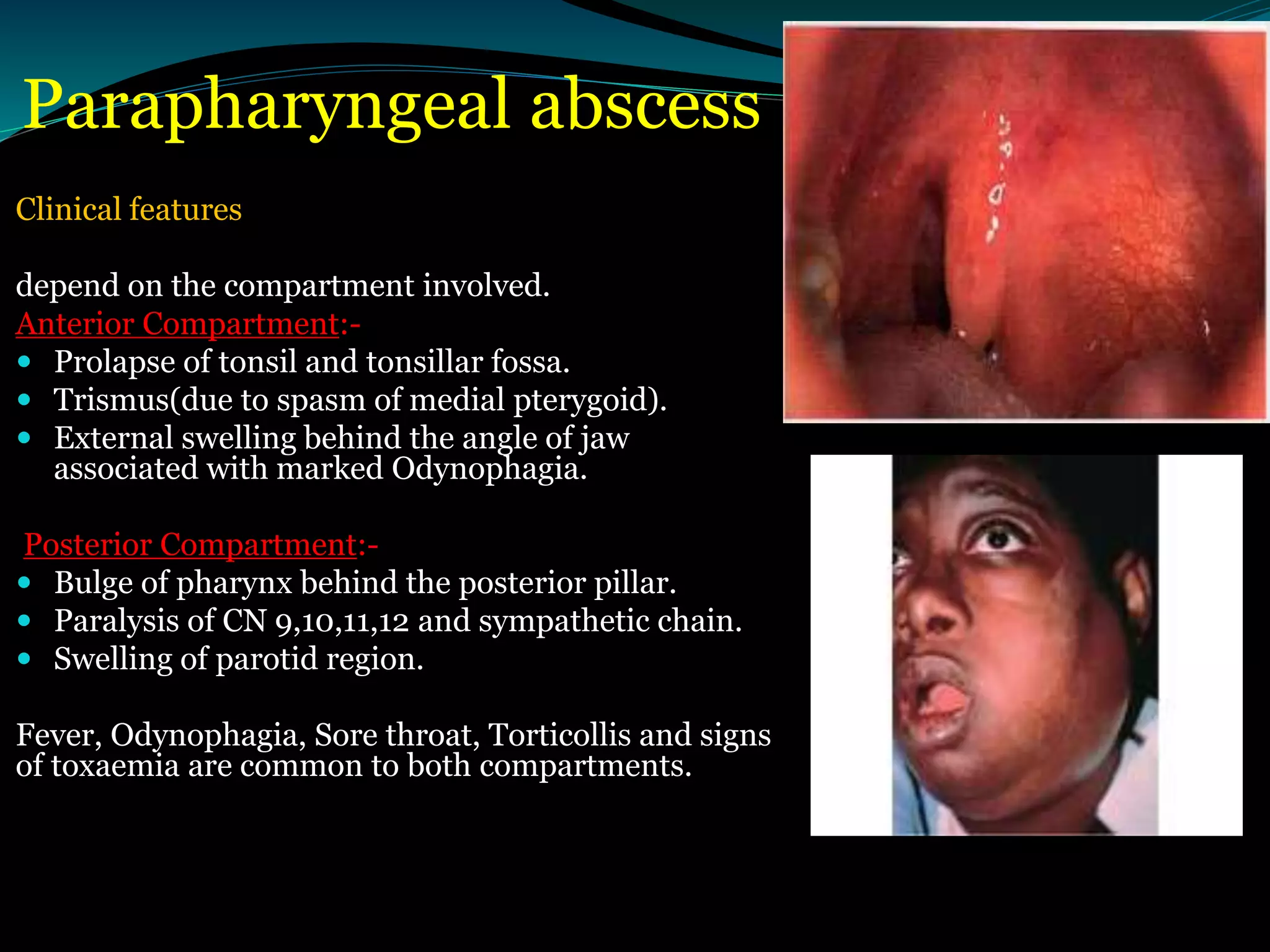
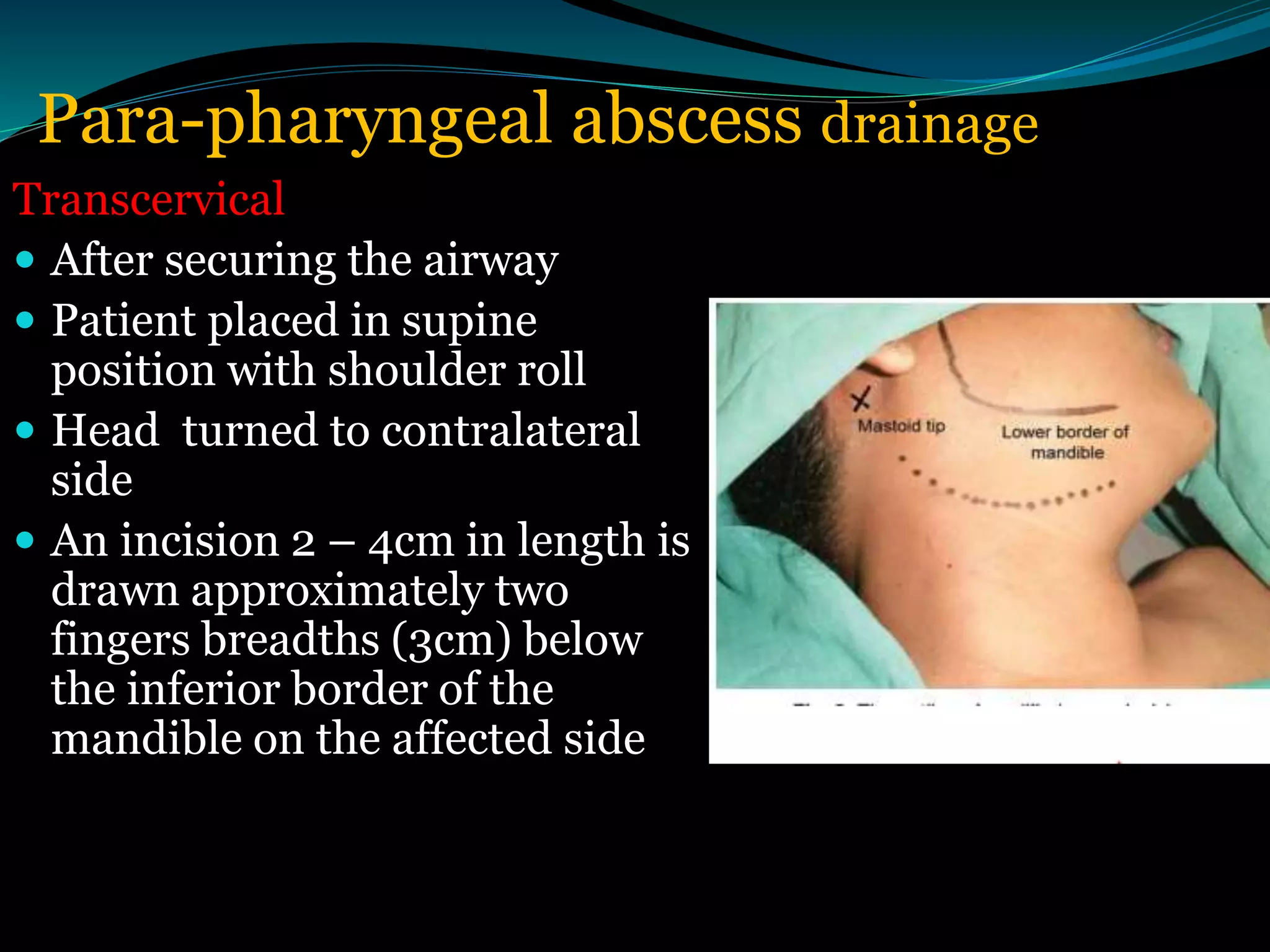
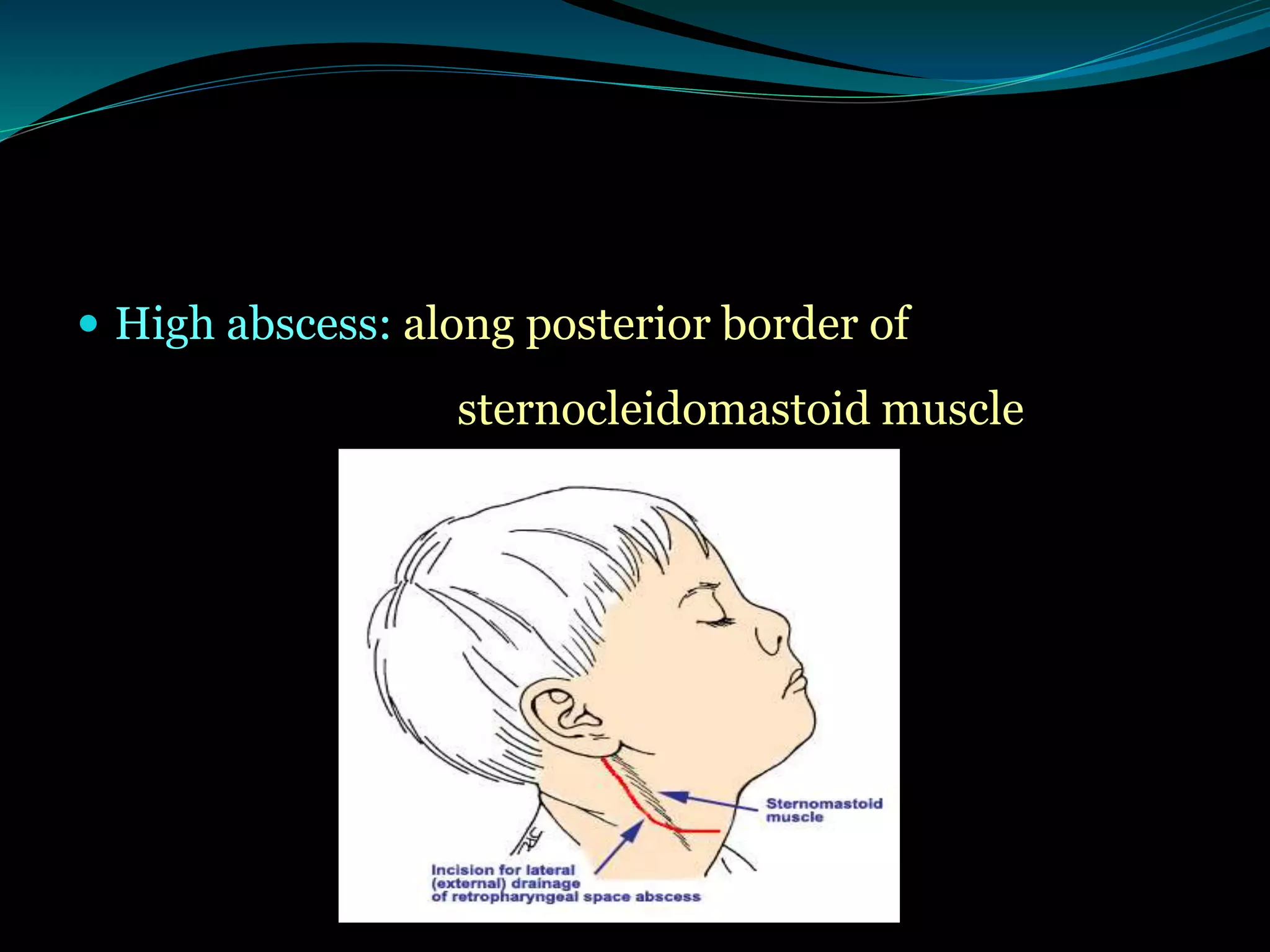
The document discusses various deep neck spaces including the parapharyngeal and retropharyngeal spaces. It describes parapharyngeal and retropharyngeal abscesses, including their etiology, clinical features, investigations, and surgical treatment which involves securing the airway followed by either a transoral or transcervical approach to drain the abscess completely while protecting nearby structures.