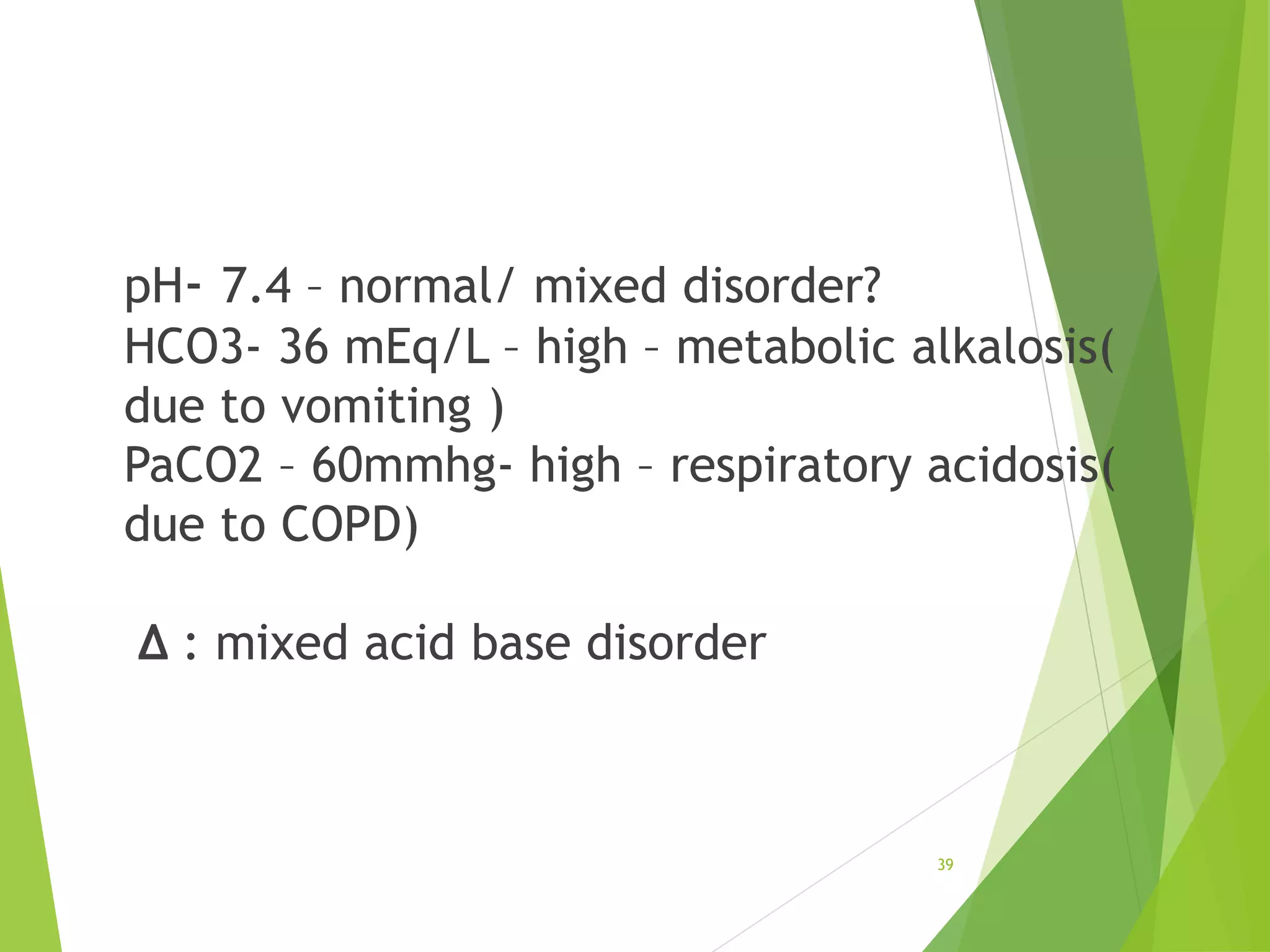
This document provides information on arterial blood gas analysis including acid-base terminology, clinical terminology criteria, the anion gap, prediction of compensatory changes, primary acid-base disorders, mixed acid-base disorders, examples of acid-base disorders, and causes of various disorders. Key points include definitions of acidemia, acidosis, alkalemia, and alkalosis. Normal values for pH, PaCO2, and HCO3 are provided. Respiratory and metabolic acidosis and alkalosis are described along with expected compensatory changes.