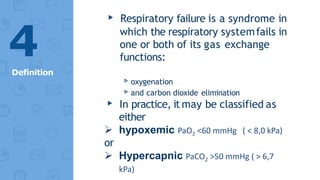
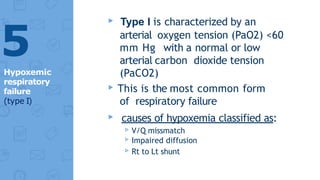
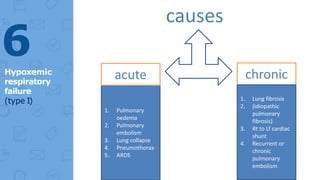
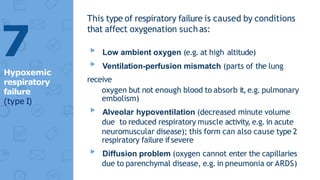
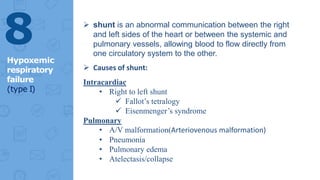
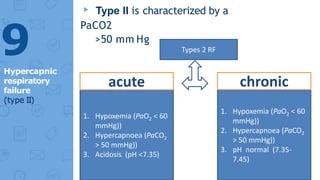
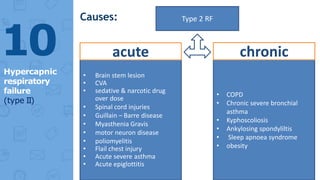
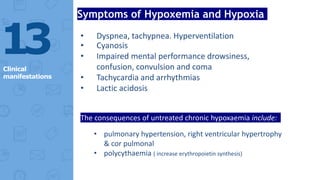
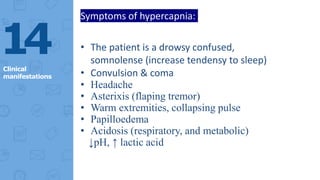
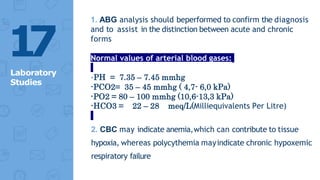
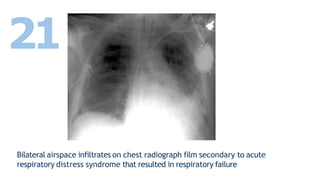
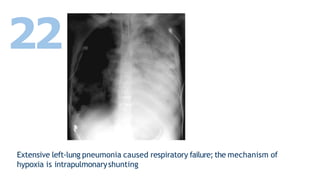
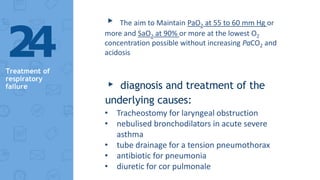
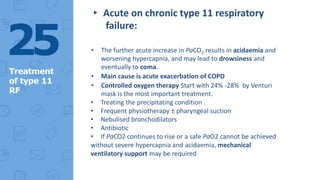
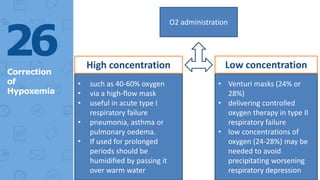
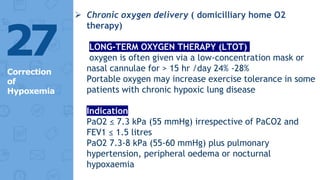
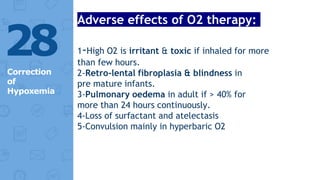
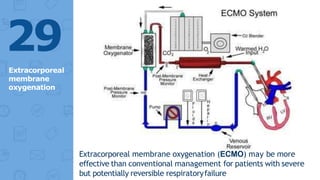
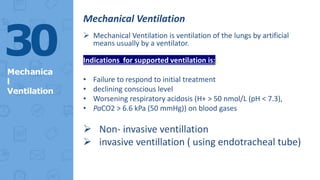
The document provides a comprehensive overview of respiratory failure, including its types (hypoxemic and hypercapnic), causes, clinical presentation, workup, and treatment approaches. It details diagnostic strategies, symptoms associated with both forms of respiratory failure, and the role of various medical interventions, including supplemental oxygen and mechanical ventilation. Emphasis is placed on early diagnosis and addressing underlying causes to effectively manage the condition.