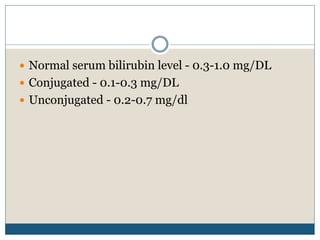
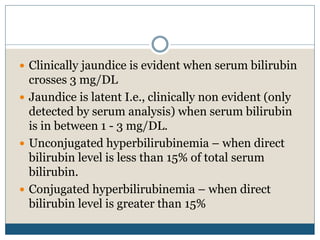
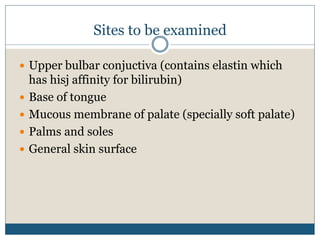
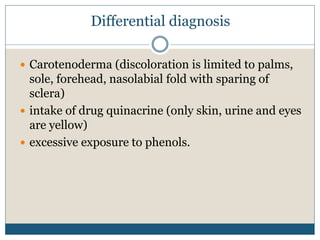
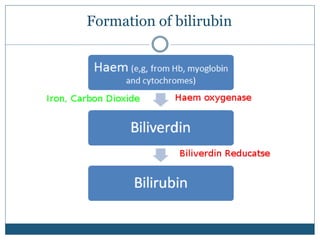
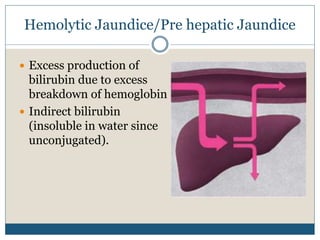
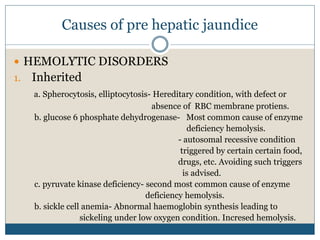
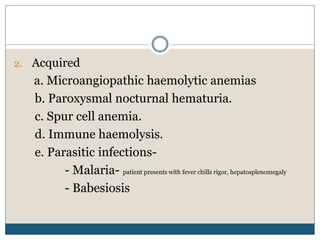
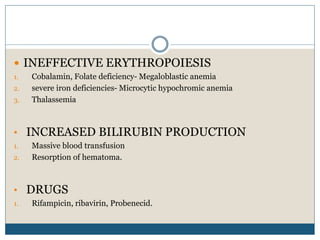
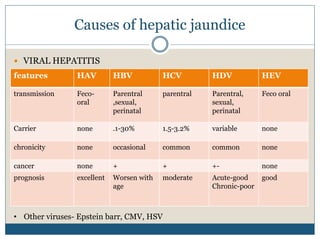
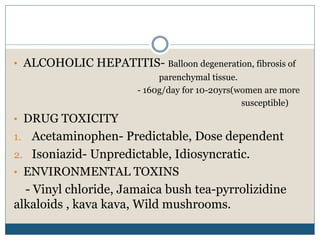
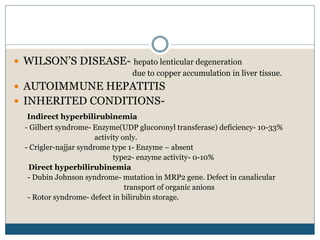
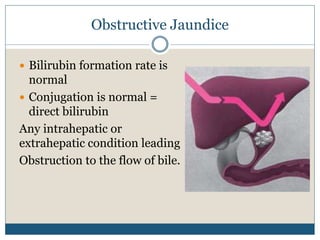
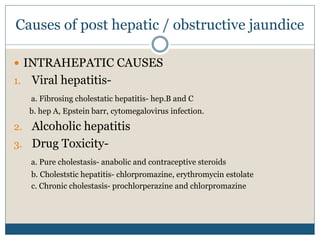
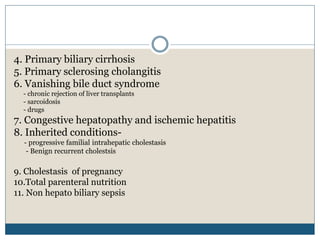
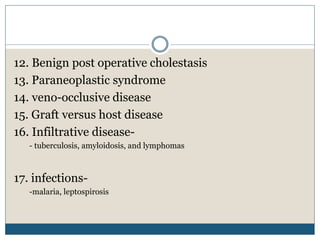
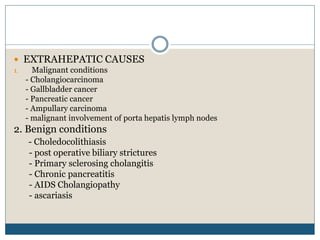
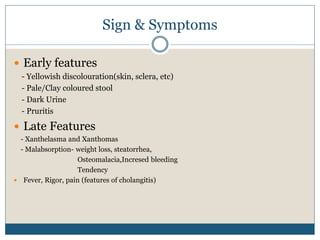
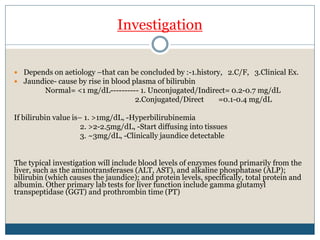
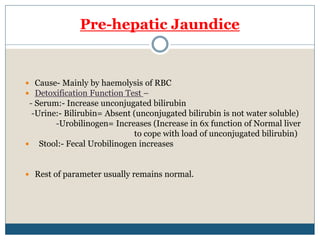
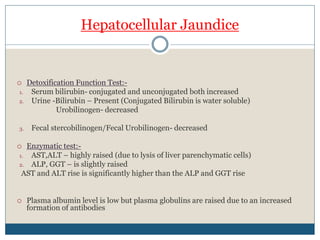
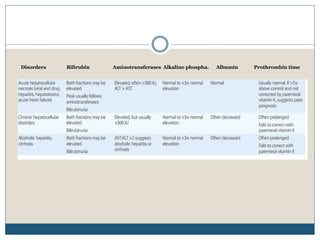
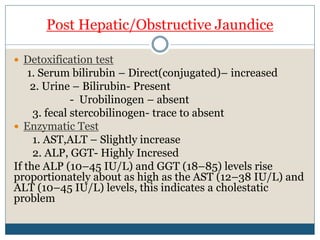
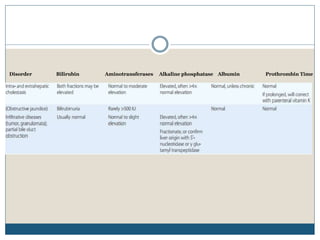
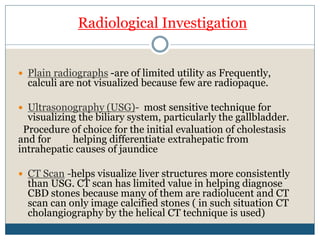
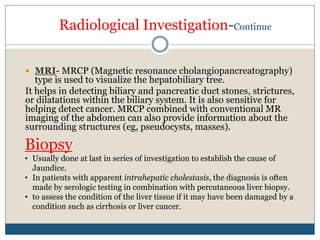
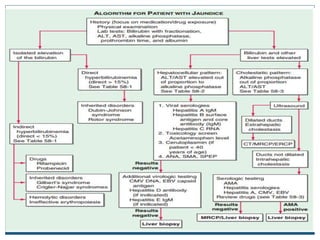
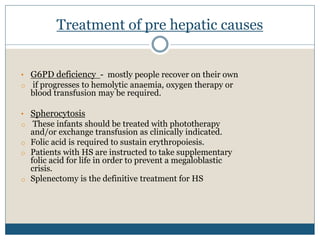
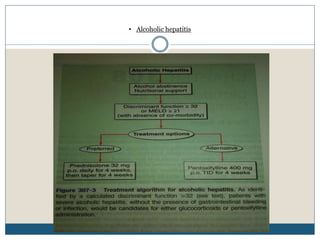
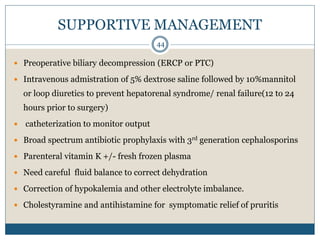
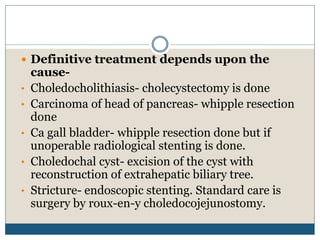
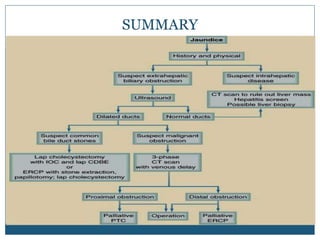
The document provides a comprehensive overview of jaundice, detailing its types (pre-hepatic, hepatic, post-hepatic), causes, symptoms, diagnosis, and treatment methods. It highlights the role of bilirubin levels in determining the type of jaundice and includes specific conditions such as viral hepatitis, hemolytic disorders, and obstructive jaundice. Treatment varies based on the etiology and encompasses supportive care, medication, and surgical options.