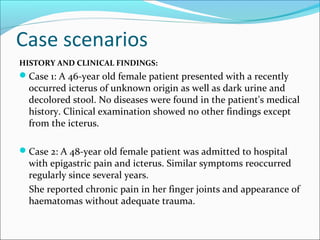
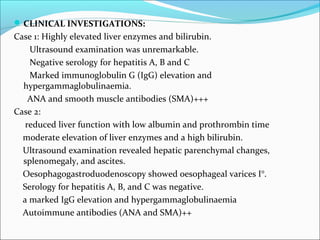
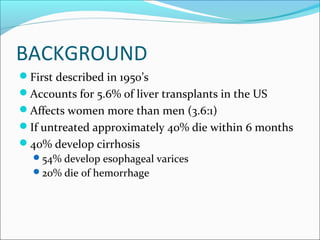
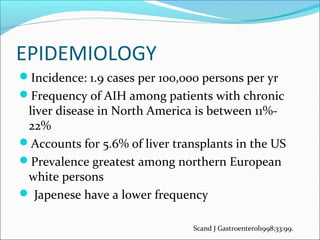
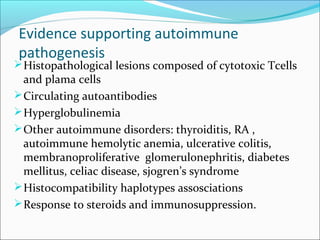
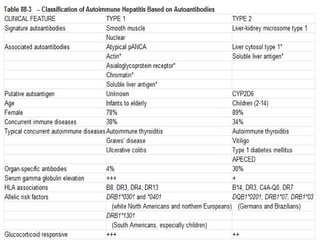
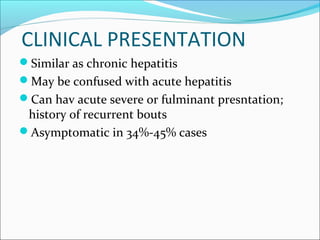
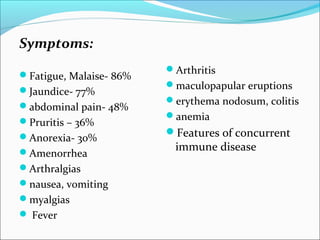
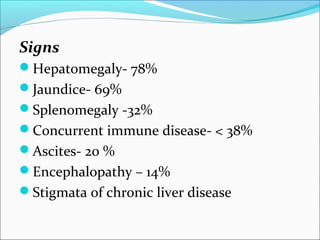
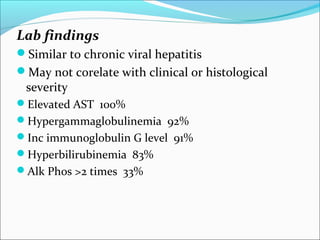
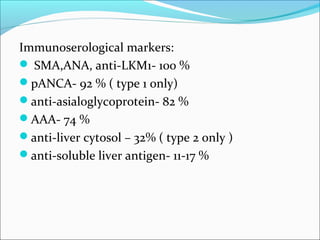
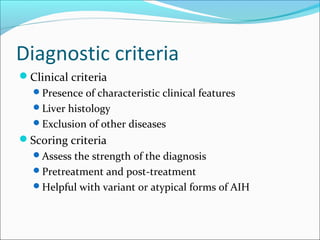
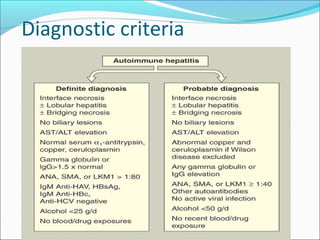
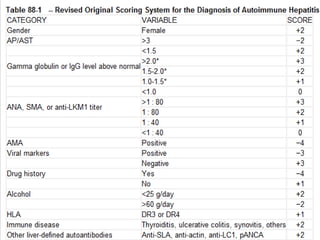
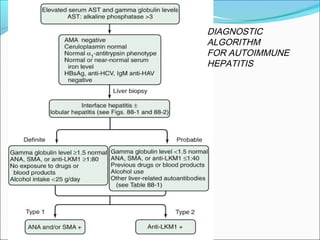
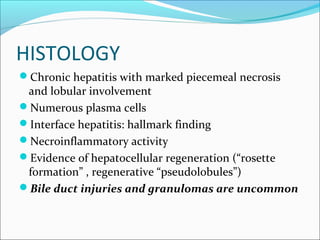
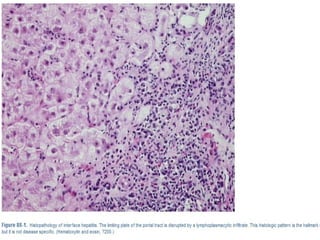
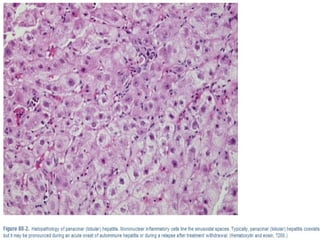
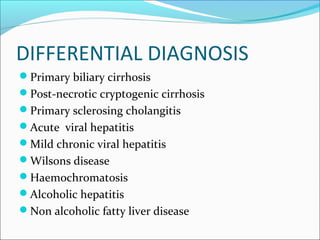
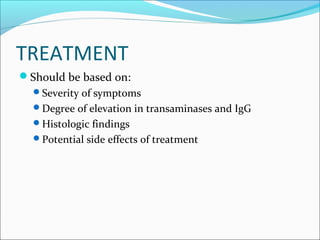
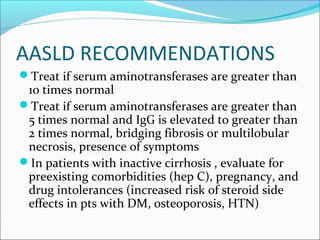
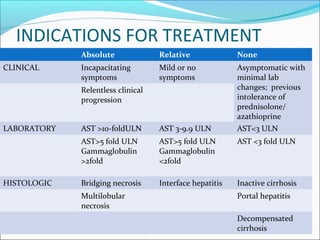
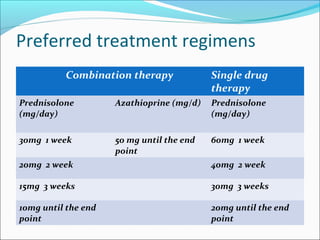
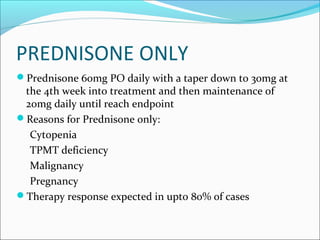
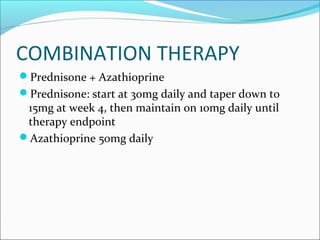
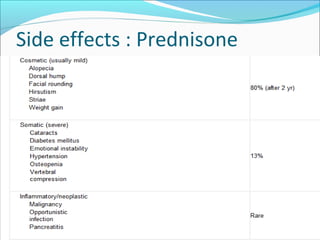
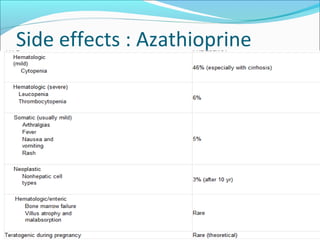
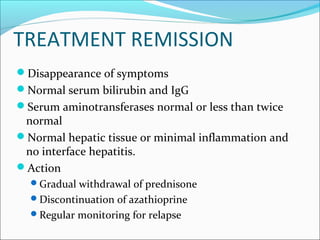
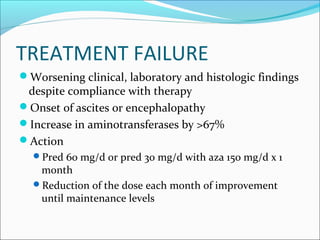
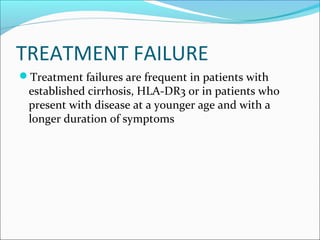
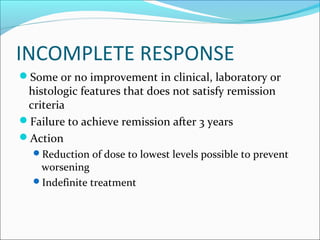
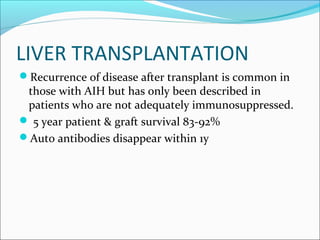
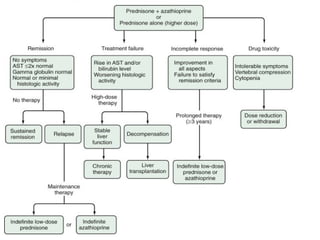
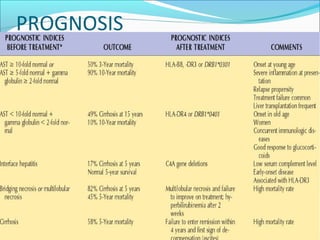
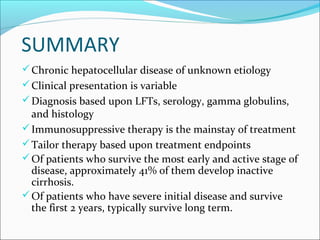
The document discusses two cases of female patients presenting with jaundice and abdominal pain. Clinical investigations found elevated liver enzymes and antibodies associated with autoimmune hepatitis. Autoimmune hepatitis is a chronic liver disease of unknown cause characterized by ongoing liver inflammation and necrosis. It can progress to cirrhosis if left untreated. The standard treatment is immunosuppressive therapy with prednisone and azathioprine to induce and maintain remission.