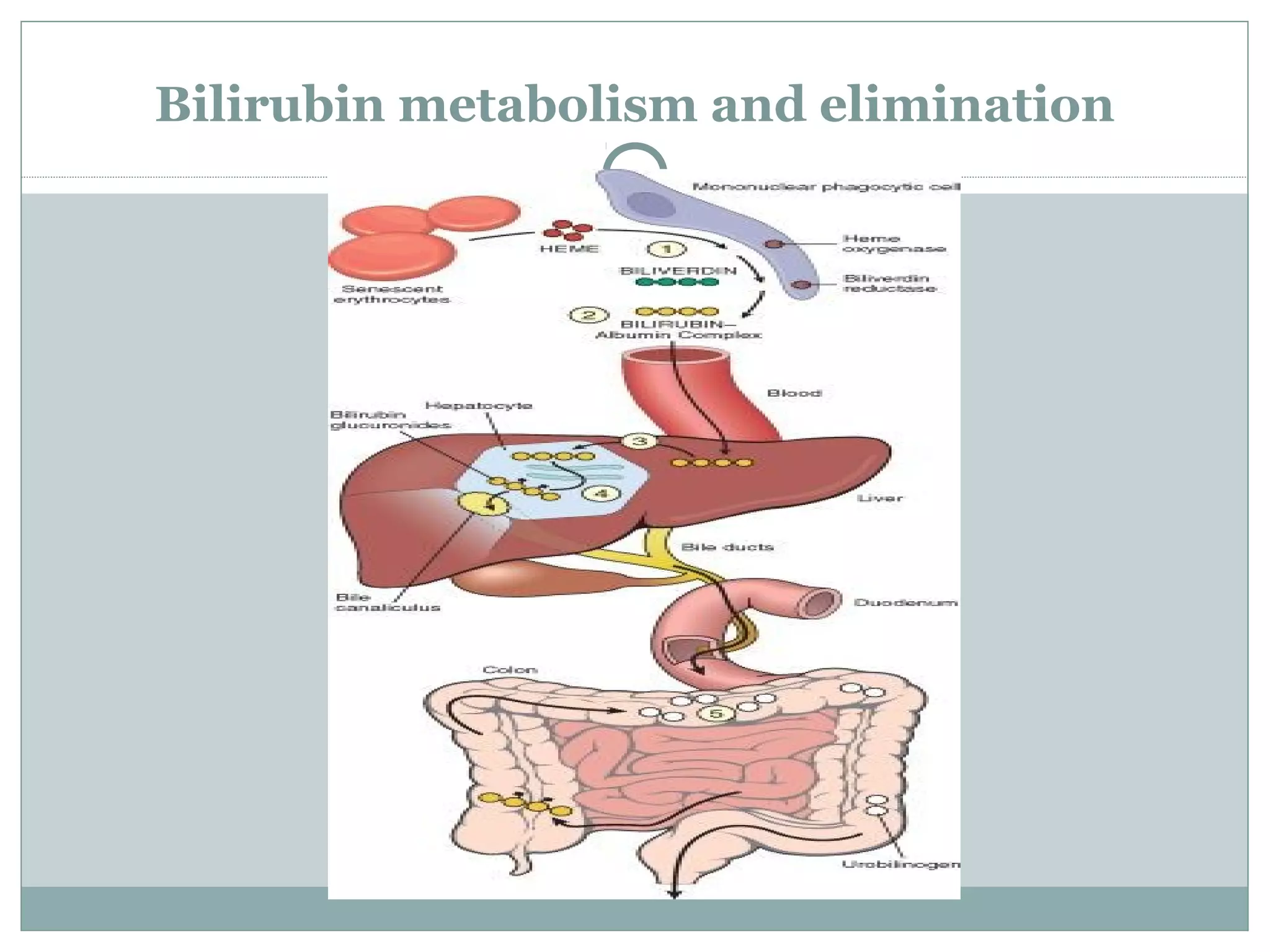
Jaundice, or icterus, refers to yellowing of the skin and eyes due to high bilirubin levels in the blood. Bilirubin is produced from the breakdown of hemoglobin and normally conjugated and excreted in bile. Jaundice can be pre-hepatic from excessive bilirubin production, hepatic from impaired conjugation or transport, or post-hepatic from bile duct obstruction. Hemolytic jaundice involves increased bilirubin from red blood cell destruction. Hepatocellular jaundice stems from liver disease impairing bilirubin excretion. Cholestatic jaundice occurs when conjugated bilirubin cannot enter bile ducts due