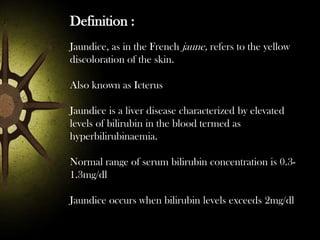
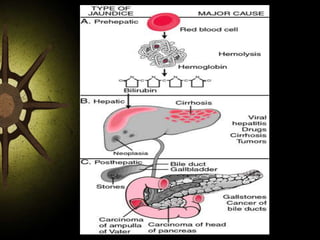
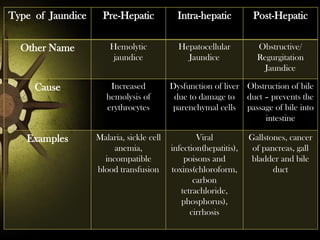
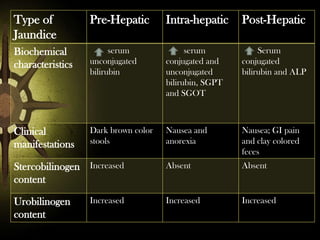
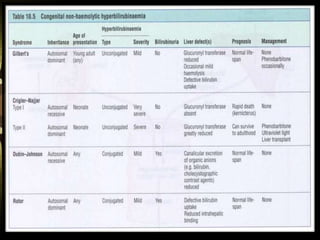
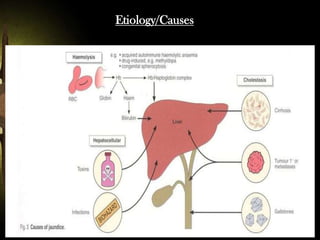
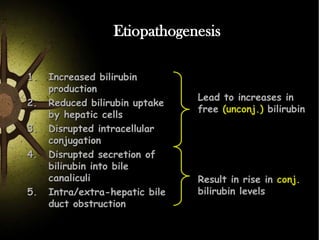
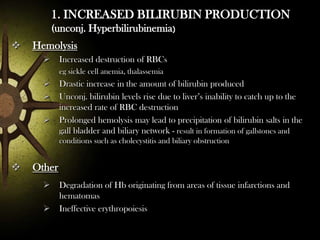
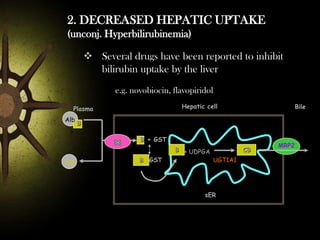
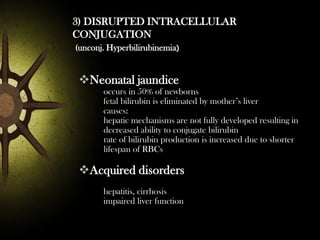
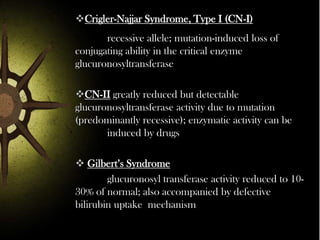
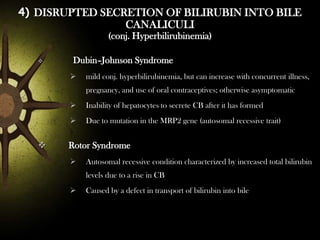
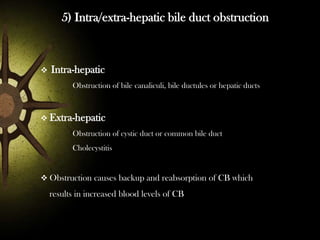
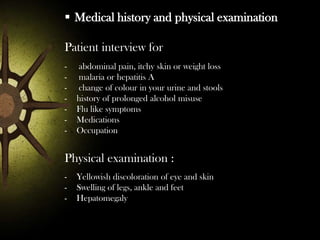
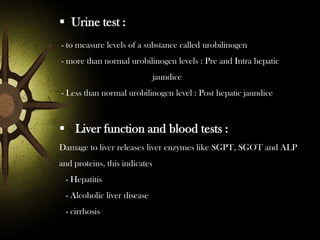
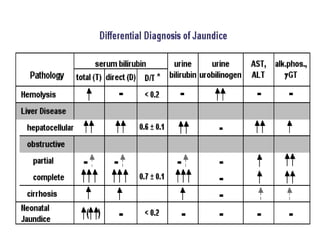
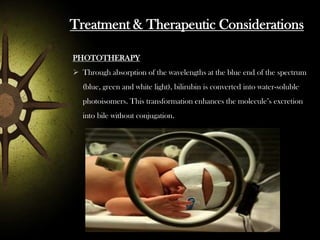
Jaundice, also known as icterus, is a liver disease characterized by elevated bilirubin levels in the blood. It occurs when bilirubin levels exceed 2mg/dl. There are three main types - prehepatic, intrahepatic, and posthepatic - depending on where the blockage of bilirubin occurs. Signs and symptoms include yellowing of the skin and eyes. Diagnosis involves medical history, physical exam, urine and blood tests, and imaging. Treatment depends on the underlying cause but may include phototherapy, medications to improve bilirubin clearance or surgery to unblock bile ducts. Prevention focuses on limiting potential liver toxins and maintaining vaccination against hepatitis viruses