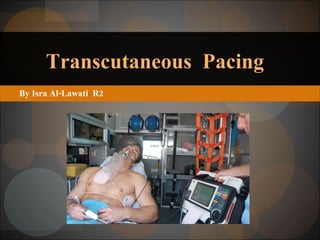
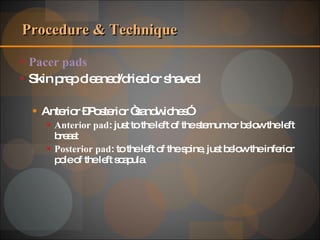
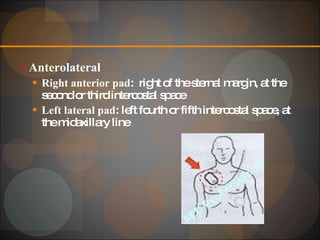
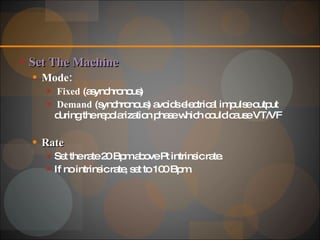
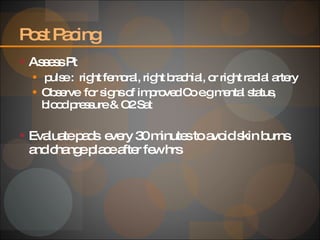
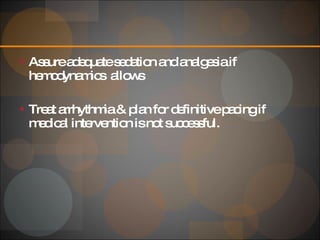
Transcutaneous pacing (TCP) uses electrical stimulation from electrode pads to induce cardiac depolarization in a rapid, safe, and non-invasive way to increase heart rate and improve cardiac output for short periods. TCP is indicated for hemodynamically significant bradydysrhythmias unresponsive to atropine or witnessed asystole. Contraindications include VF, awake and stable patients, and severe hypothermia. The procedure involves preparing the skin and placing anterior-posterior pads on the chest to deliver electrical impulses from an external pacer to capture the heart rhythm. Complications can include failure to detect VF, inducing arrhythmias, pain, or skin burns.