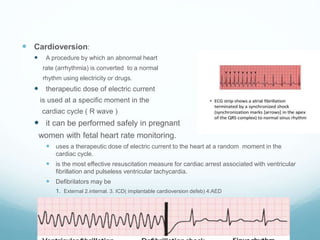
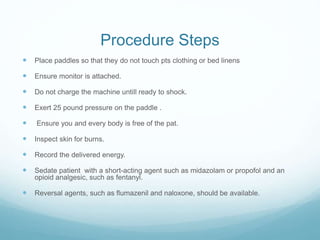
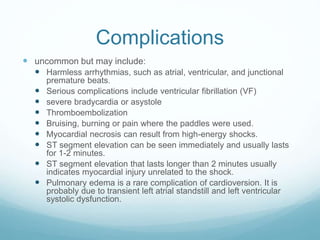
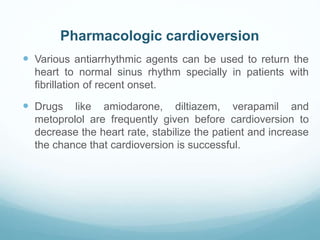
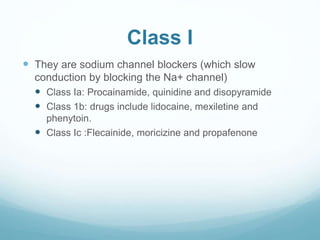
Cardioversion is a procedure that uses electric shock or drugs to convert an abnormal heart rhythm back to normal. There are two main types - electrical cardioversion, which delivers a synchronized electric shock, and pharmacological cardioversion, which uses antiarrhythmic drugs. Electrical cardioversion can be elective or emergency, while pharmacological cardioversion utilizes various classes of drugs like beta blockers, sodium channel blockers, and calcium channel blockers to restore normal rhythm. The document outlines the differences between cardioversion and defibrillation, indications and contraindications for cardioversion, recommendations, procedure steps, complications, and drug options for pharmacological cardioversion.