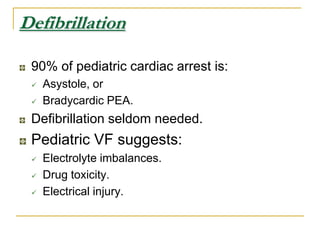
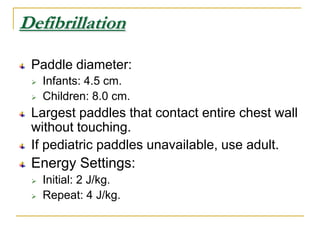
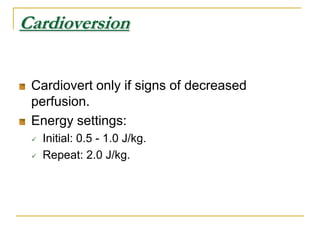
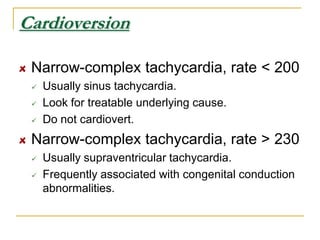
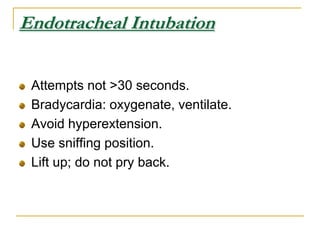
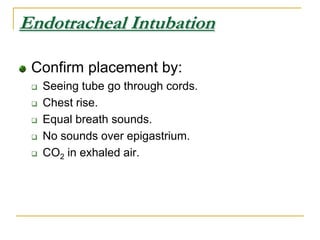
This document discusses resuscitation in special populations, including pediatrics and pregnant women. In pediatrics, the most important interventions are oxygenation and ventilation due to respiratory causes being common in pediatric cardiac arrest. Anatomy differs from adults with a relatively larger head, more anterior larynx, and narrower airway. Resuscitation techniques are modified for pediatrics, such as using two fingers for infant chest compressions. In pregnancy, the uterus presses on major vessels so resuscitation focuses on maternal survival to benefit the fetus. Left lateral positioning and early airway management are important, and chest compressions are performed higher on the sternum. Emergency c-section within 5 minutes of cardiac arrest may improve infant outcomes

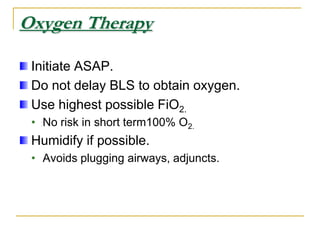
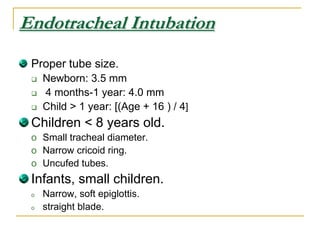
![Oxygen TherapyInitiate ASAP. Do not delay BLS to obtain oxygen.Use highest possible FiO2.No risk in short term100% O2.Humidify if possible.Avoids plugging airways, adjuncts.Endotracheal IntubationProper tube size.Newborn: 3.5 mm 4 months-1 year: 4.0 mmChild > 1 year: [(Age + 16 ) / 4]Children < 8 years old.Small tracheal diameter.](https://image.slidesharecdn.com/resuscitationinspecialpopulations-100907031126-phpapp02/85/Resuscitation-in-special-populations-17-320.jpg)