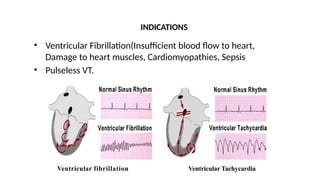
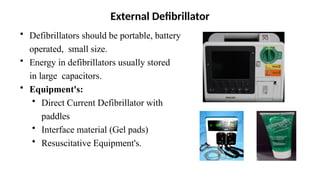
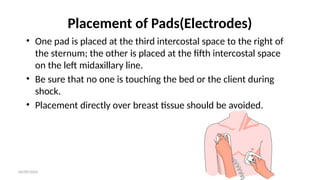
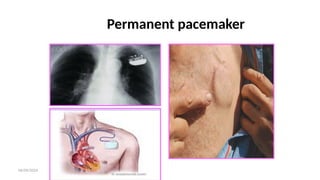
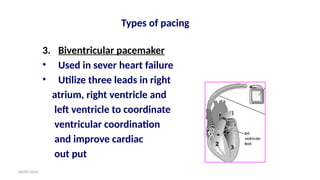
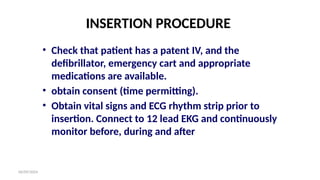
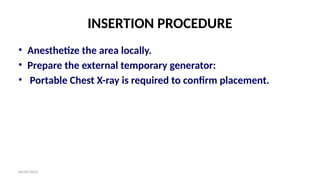
Defibrillation is a lifesaving process where a defibrillator delivers an electric shock to the heart to restore normal rhythm, particularly in cases of ventricular fibrillation. Various types of defibrillators exist, such as automated external defibrillators and implantable cardioverter-defibrillators, each designed for different situations and users. Proper procedure for defibrillation and pacemaker insertion includes clear steps for CPR, electrode placement, and post-care responsibilities, emphasizing the importance of monitoring and patient education regarding the device's use and safety.