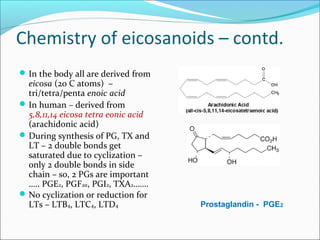
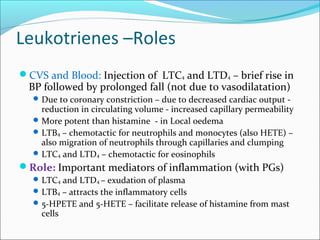
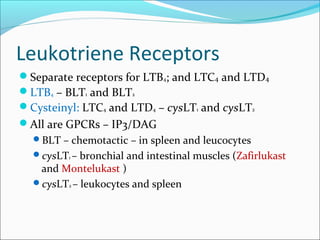
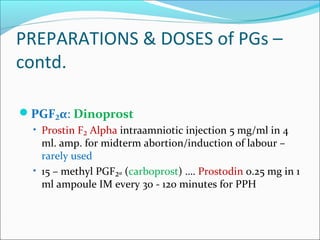
The document discusses prostaglandins (PGs) and leukotrienes (LTs), essential fatty acid-derived autacoids with local hormone-like functions in various bodily tissues. It outlines their biosynthesis, types, roles in physiological processes, therapeutic applications, and mechanisms of action. Additionally, it covers the pathophysiological roles of these eicosanoids in cardiovascular, gastrointestinal, respiratory, and reproductive systems, including their implications in inflammation and pain regulation.