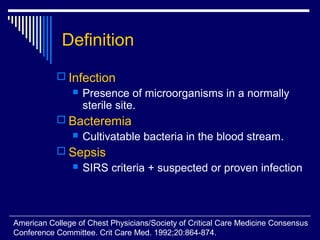
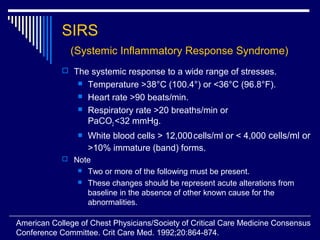
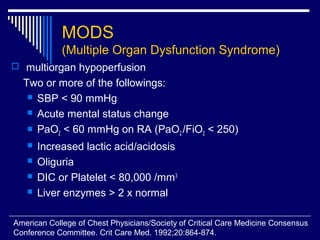
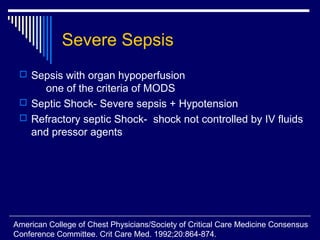
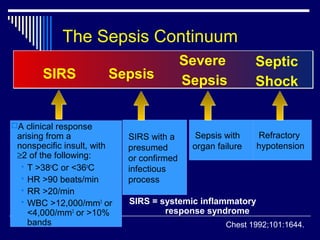
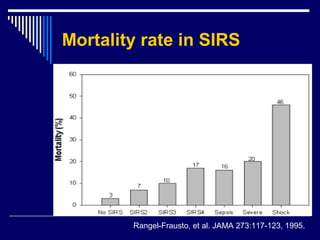
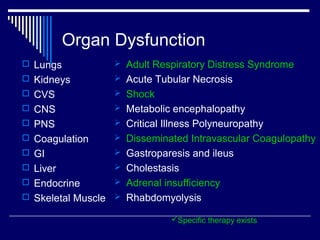
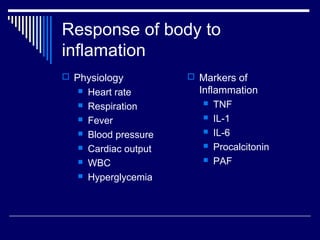
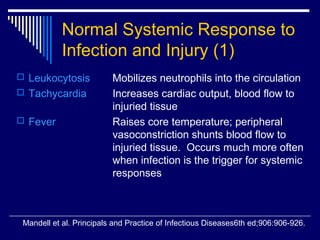
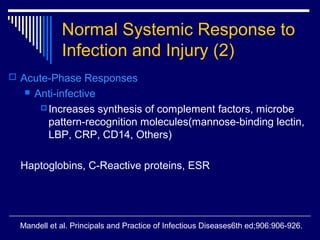
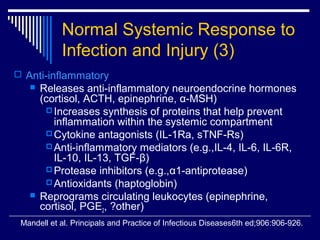
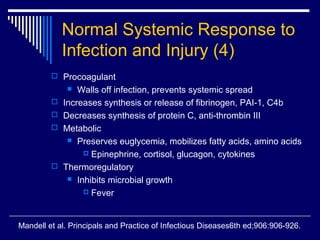
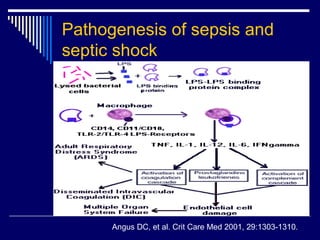
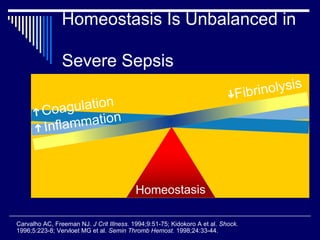
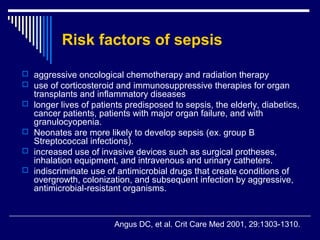
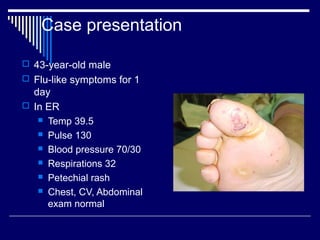
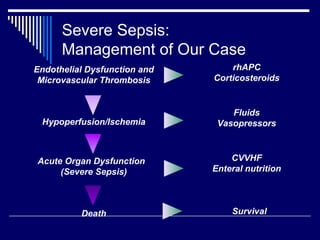
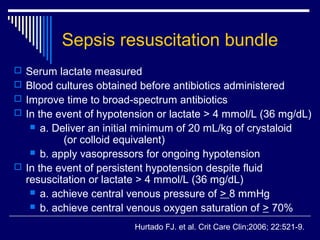
The document discusses systemic inflammatory response syndrome (SIRS) and defines it as a systemic response to various stresses that includes symptoms like fever, increased heart rate, respiratory rate and white blood cell count. It outlines the progression from infection to bacteremia to sepsis, which involves SIRS criteria and a suspected or proven infection. The stages of sepsis like severe sepsis, septic shock and refractory septic shock are defined based on the presence of organ dysfunction or hypotension.