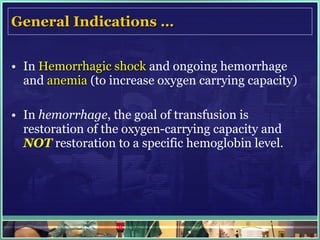
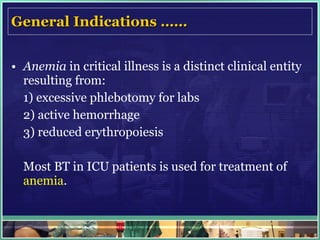
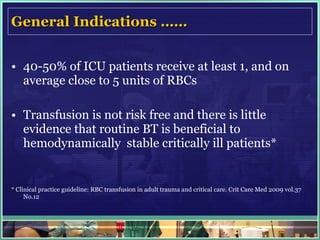
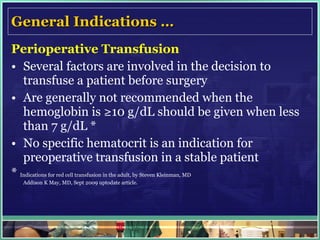
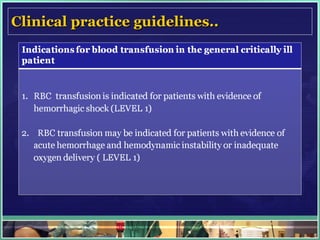
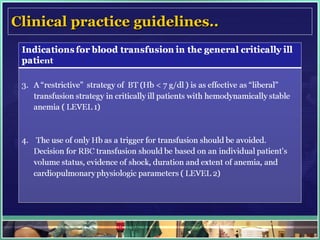
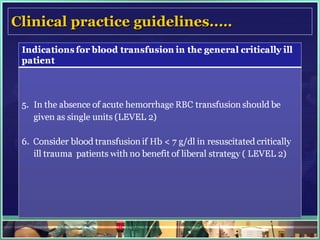
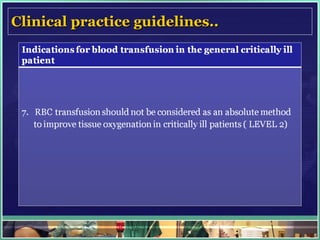
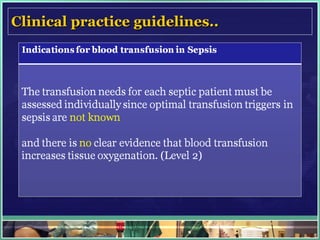
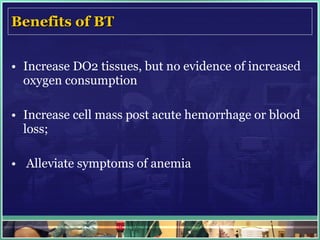
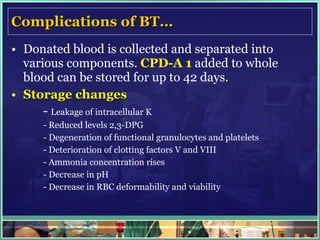
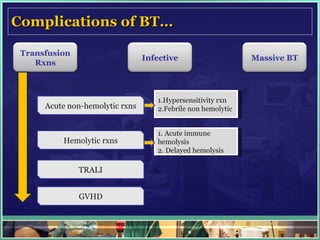
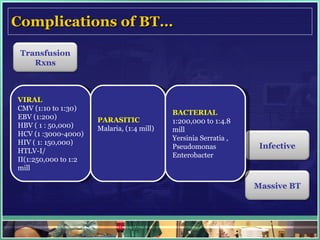
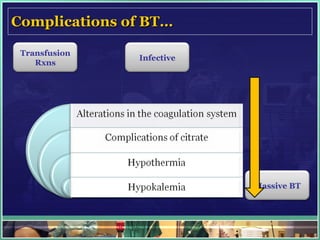
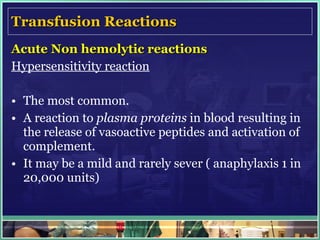
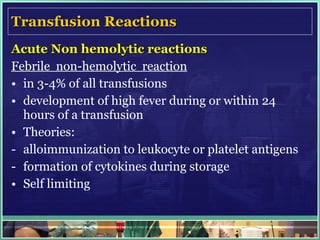
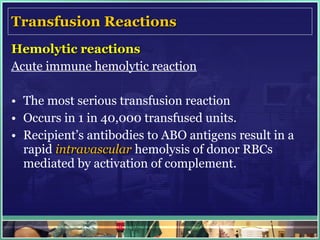
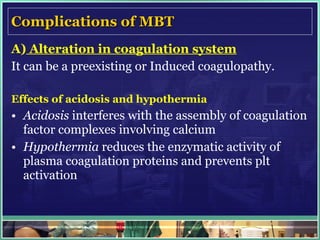
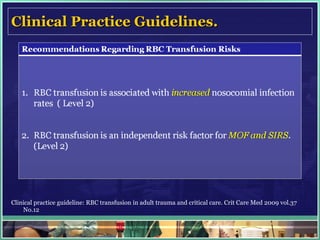
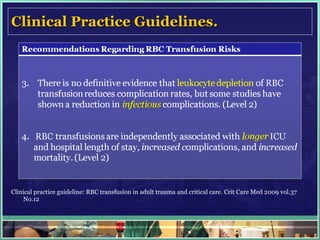
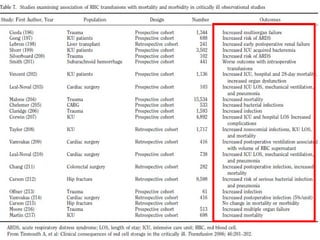
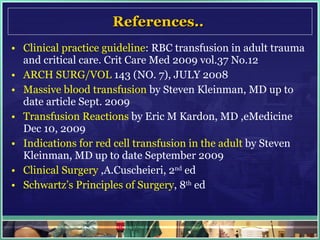
This document defines massive blood transfusion as replacing over half the patient's blood volume within 24 hours or transfusing over 10 units of packed red blood cells within a few hours. It indicates massive transfusion is used for hemorrhagic shock, trauma, or critical illness. Complications discussed include acute reactions, infections transmission, coagulopathy, hypothermia, electrolyte abnormalities, and volume overload. Guidelines recommend considering multiple factors like physiological status and oxygen needs rather than single transfusion thresholds.