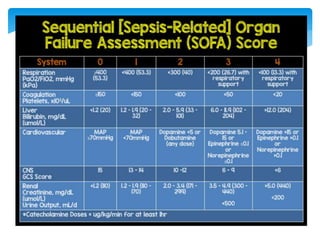
This document discusses shock, specifically endotoxic shock. It begins with definitions of terms like shock, sepsis, and systemic inflammatory response syndrome. It then classifies and describes the different types of shock: hypovolaemic, distributive, obstructive, and cardiogenic. The main focus is on the pathophysiology and management of septic shock. It discusses the circulatory dysfunction that occurs in sepsis and leads to shock. The clinical features, evaluation, and treatment principles including hemodynamic support, fluids, vasopressors, inotropes, antimicrobial therapy, and surgery are covered. Prevention and prognosis of septic shock are also mentioned.