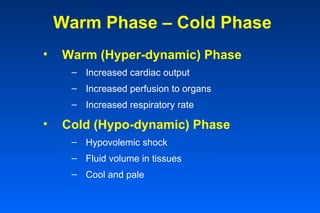
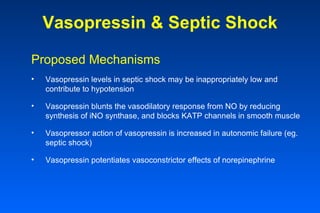
Sepsis is a systemic inflammatory response to infection that can lead to organ dysfunction and death. It is a major cause of death in intensive care units. The incidence of sepsis is rising due to an aging population and increased use of invasive medical procedures and devices. Sepsis progresses through a spectrum from systemic inflammatory response syndrome to severe sepsis with organ dysfunction to septic shock with hypotension and perfusion abnormalities if not treated promptly.