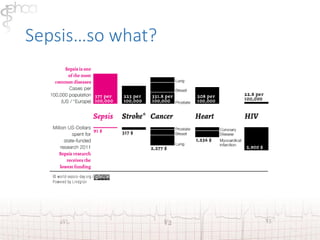
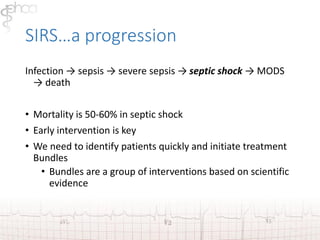
Sepsis is a life-threatening condition that arises when the body's response to infection causes injury to its own tissues. Globally, sepsis kills about 8 million people annually. Early recognition and treatment are key to improving outcomes. The first hours after diagnosis are especially critical, as mortality increases by about 8% every hour that antibiotics are delayed. Prompt administration of broad-spectrum antibiotics and fluid resuscitation can significantly reduce mortality from sepsis.

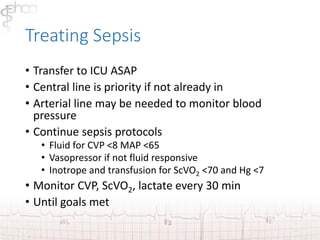
![Septic Shock
• Is acute circulatory failure unexplained by other
causes
• Patient has persistent arterial hypotension SBP<90
[MAP <60] despite adequate volume resuscitation
• Patients don’t always look “sick” until this point](https://image.slidesharecdn.com/sepsispresentationab-141024111940-conversion-gate01/85/Sepsis-12-320.jpg)

![Glucose Control
• Hyperglycemia and insulin resistance occur in severe sepsis.
• Tight glucose control with insulin is used to maintain blood
glucose 6.5-10 mmol/L [120-180 mg/dl]
• Hypoglycemia has shown to cause higher mortality in critical
patients.
• Insulin protocols should be followed.](https://image.slidesharecdn.com/sepsispresentationab-141024111940-conversion-gate01/85/Sepsis-54-320.jpg)