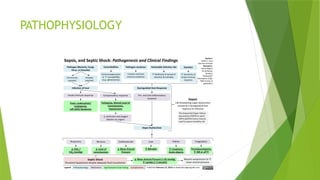
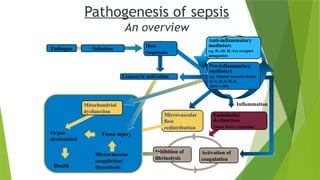
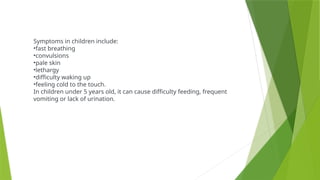
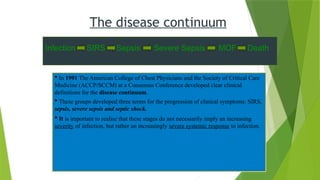
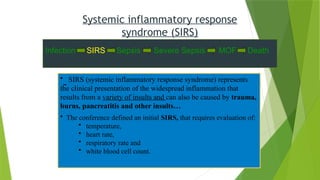
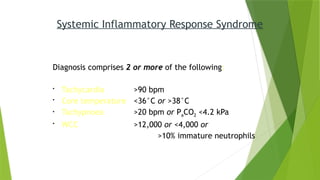
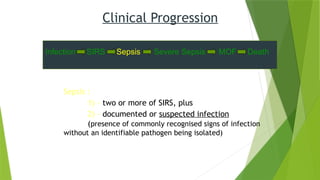
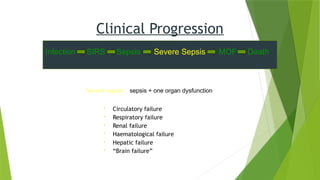
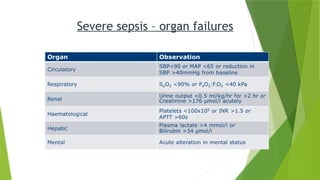
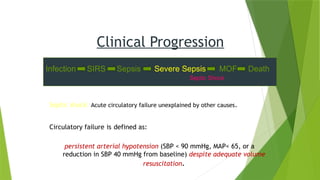
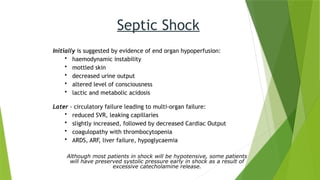
Sepsis is a life-threatening condition characterized by a systemic inflammatory response to infection, leading to potential organ dysfunction and high mortality rates, particularly in children and lower-middle-income countries. The document details the pathophysiology, clinical progression, and management strategies associated with sepsis, highlighting the importance of early recognition and intervention. It outlines the stages of sepsis, including systemic inflammatory response syndrome, sepsis, severe sepsis, and septic shock, along with the corresponding signs, symptoms, and risk factors.