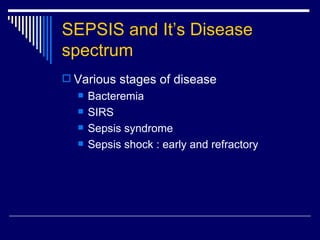
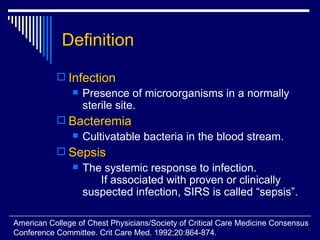
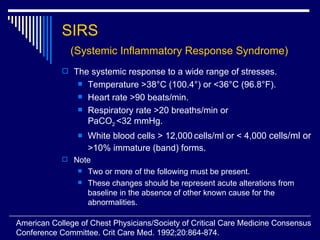
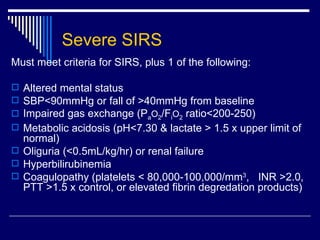
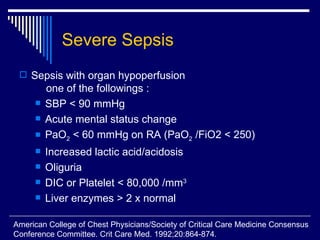
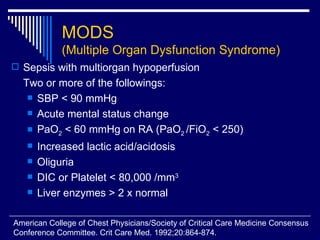
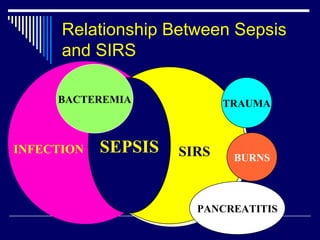
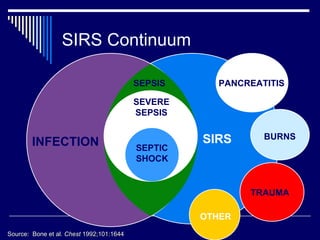
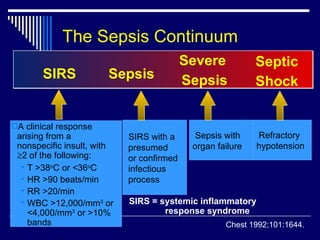
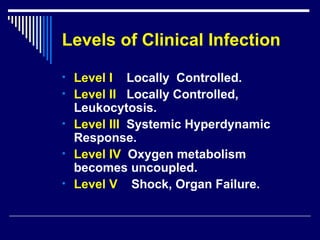
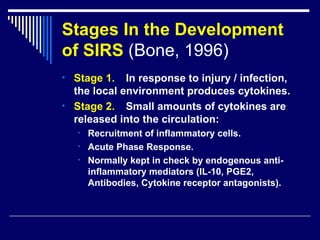
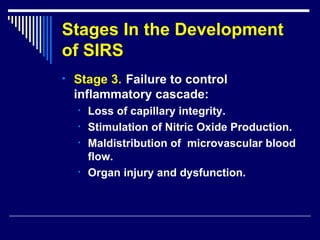
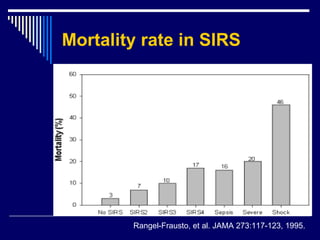
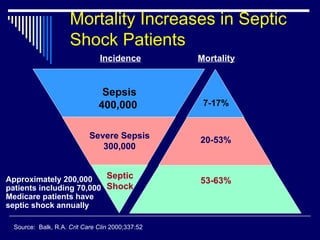
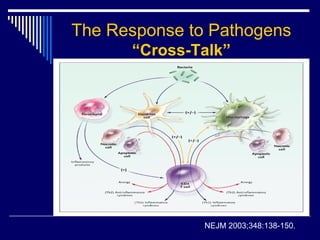
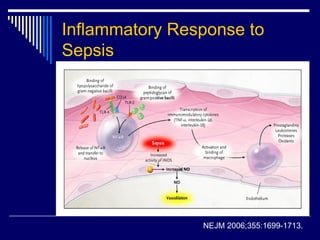
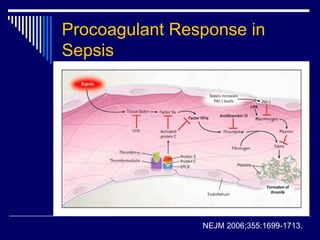
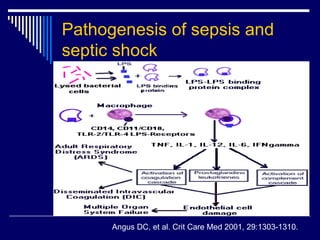
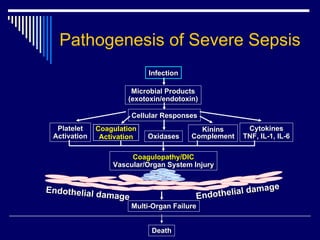
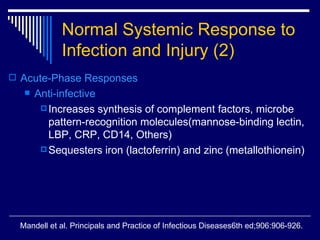
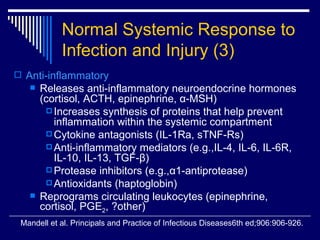
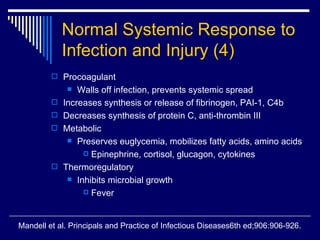
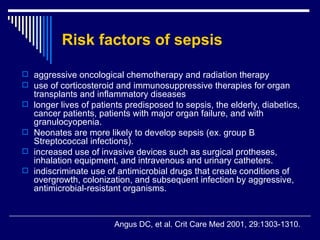
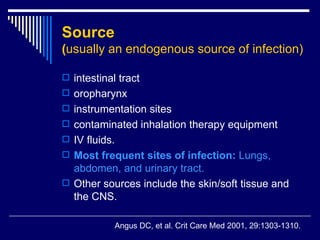
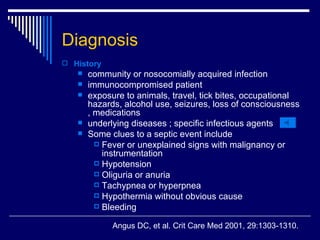
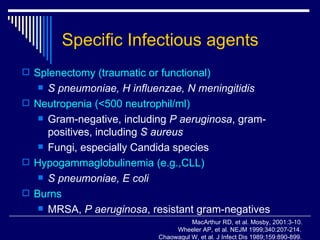
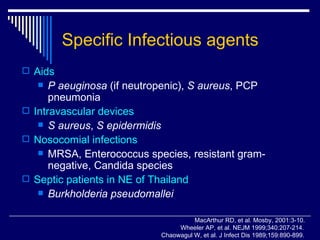
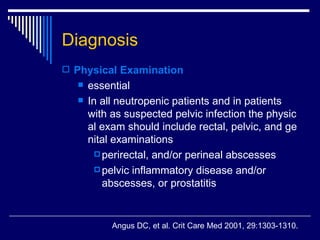
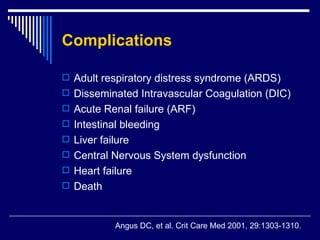
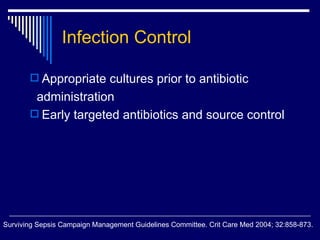
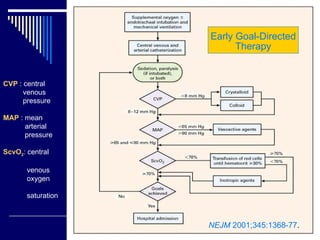
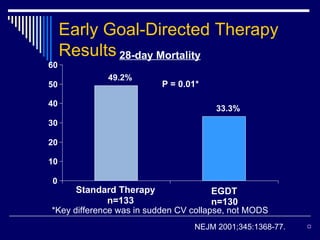
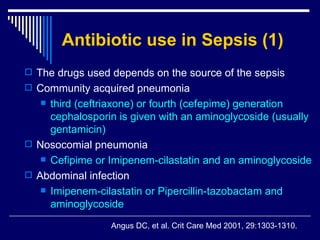
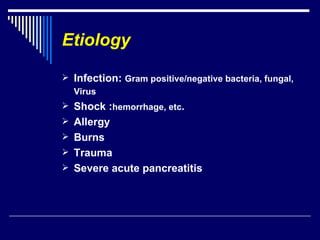
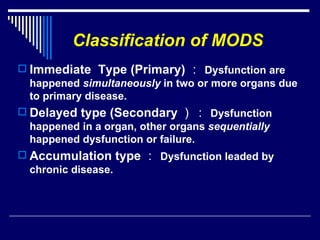
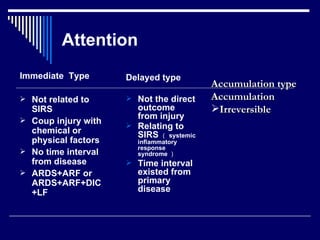
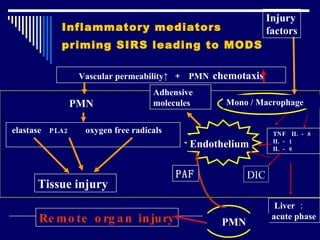
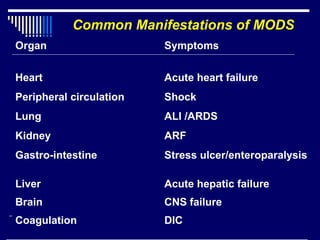
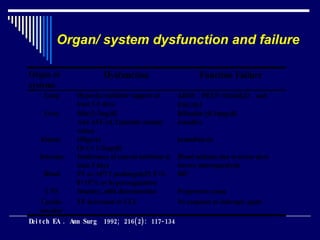
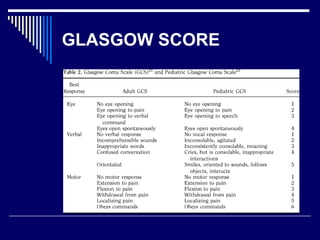
The document discusses systemic inflammatory response syndrome (SIRS) and its relationship to sepsis. It defines SIRS as a systemic response to various stresses and outlines its diagnostic criteria. SIRS can progress to sepsis if an infection is involved. Sepsis is defined as a systemic response to infection along with signs of organ dysfunction. More severe stages include severe sepsis and septic shock. Risk factors, sources of infection, and specific infectious agents associated with sepsis are also reviewed.