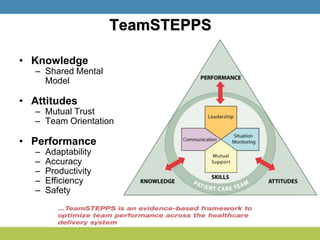
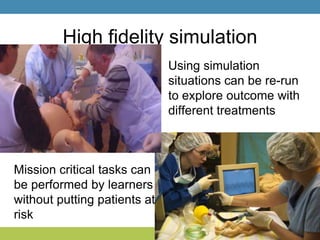
Simulation training is essential in high-risk fields like medicine, where on-the-job training can be costly or dangerous. It provides structured learning opportunities, improves crisis management, and enhances teamwork, which are crucial for reducing medical errors and improving patient outcomes. The future of simulation lies in its application across various disciplines for skills training, decision-making, and inter-professional communication.