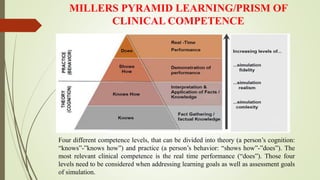
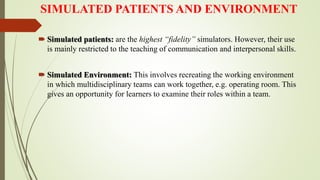
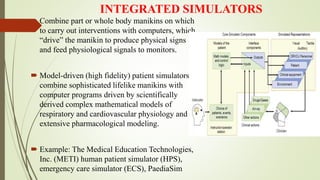
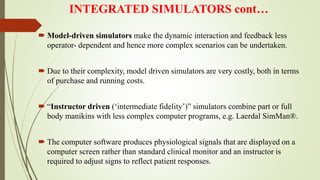
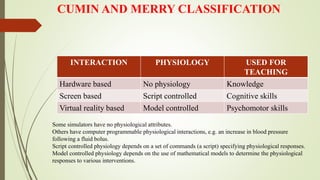
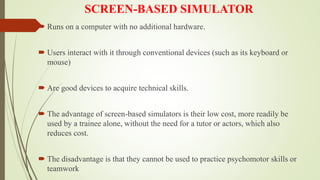
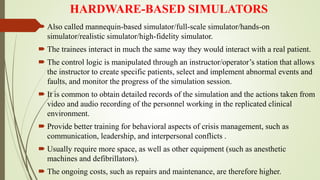
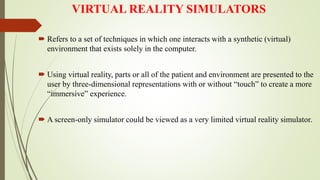
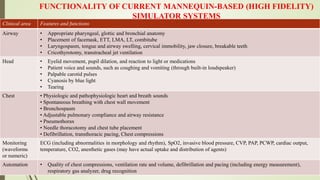
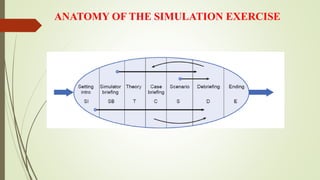
The document discusses simulation in medicine and its advantages. It describes Miller's pyramid of learning and the history of medical simulation. Simulation allows trainees to practice skills in a safe environment without risk to patients. It also allows rare scenarios to be replicated for learning. Current simulators range from part-task trainers to high-fidelity full-body mannequins that can replicate physical signs and physiological responses. The highest level of simulation incorporates simulated patients and environments to train technical and non-technical skills.