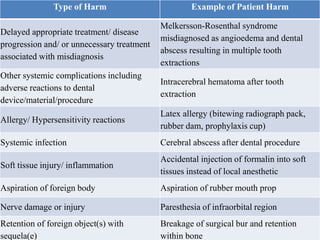
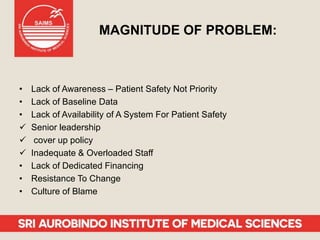
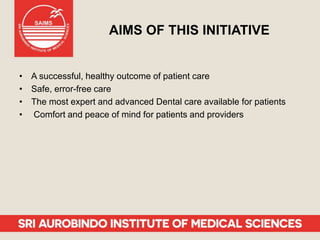
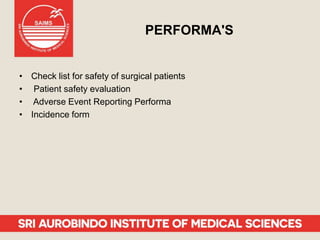
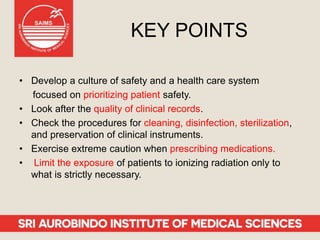
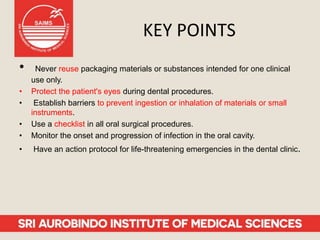
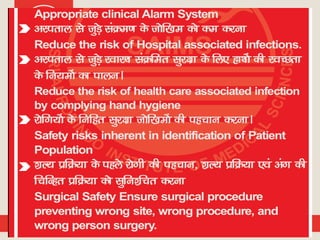
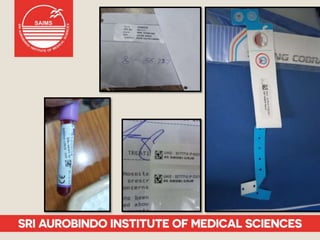
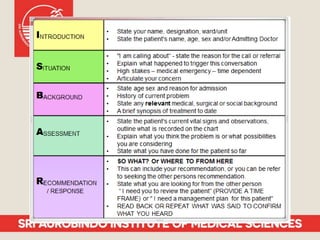
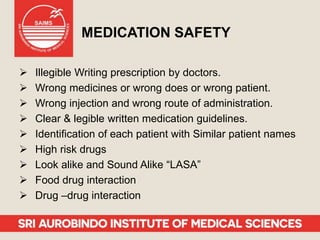
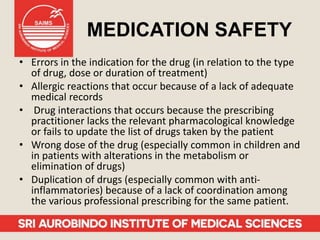
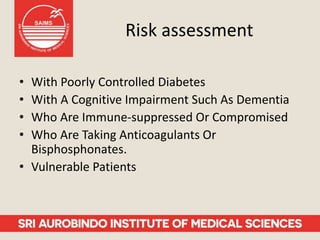
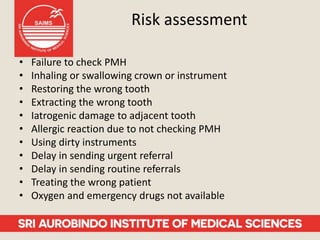
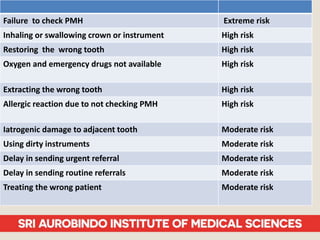
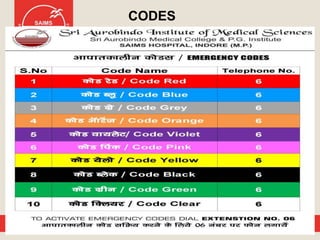
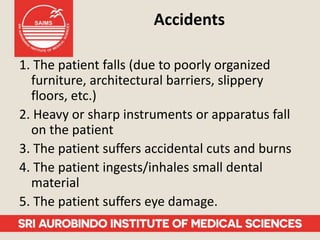
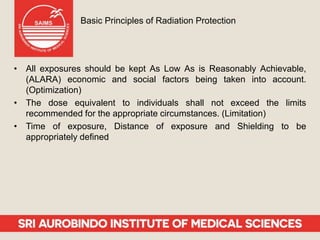
Patient safety is an important part of healthcare. It aims to prevent harm caused by accidents, errors, and complications during treatment. Some key aspects of ensuring patient safety include accurate patient identification, effective communication of medical information, safe medication practices, reducing risks of infections, conducting risk assessments, following safety protocols for radiation and surgery, and maintaining a safe clinic environment. Organizations are working to promote a culture of safety and establish systems to safeguard patients.