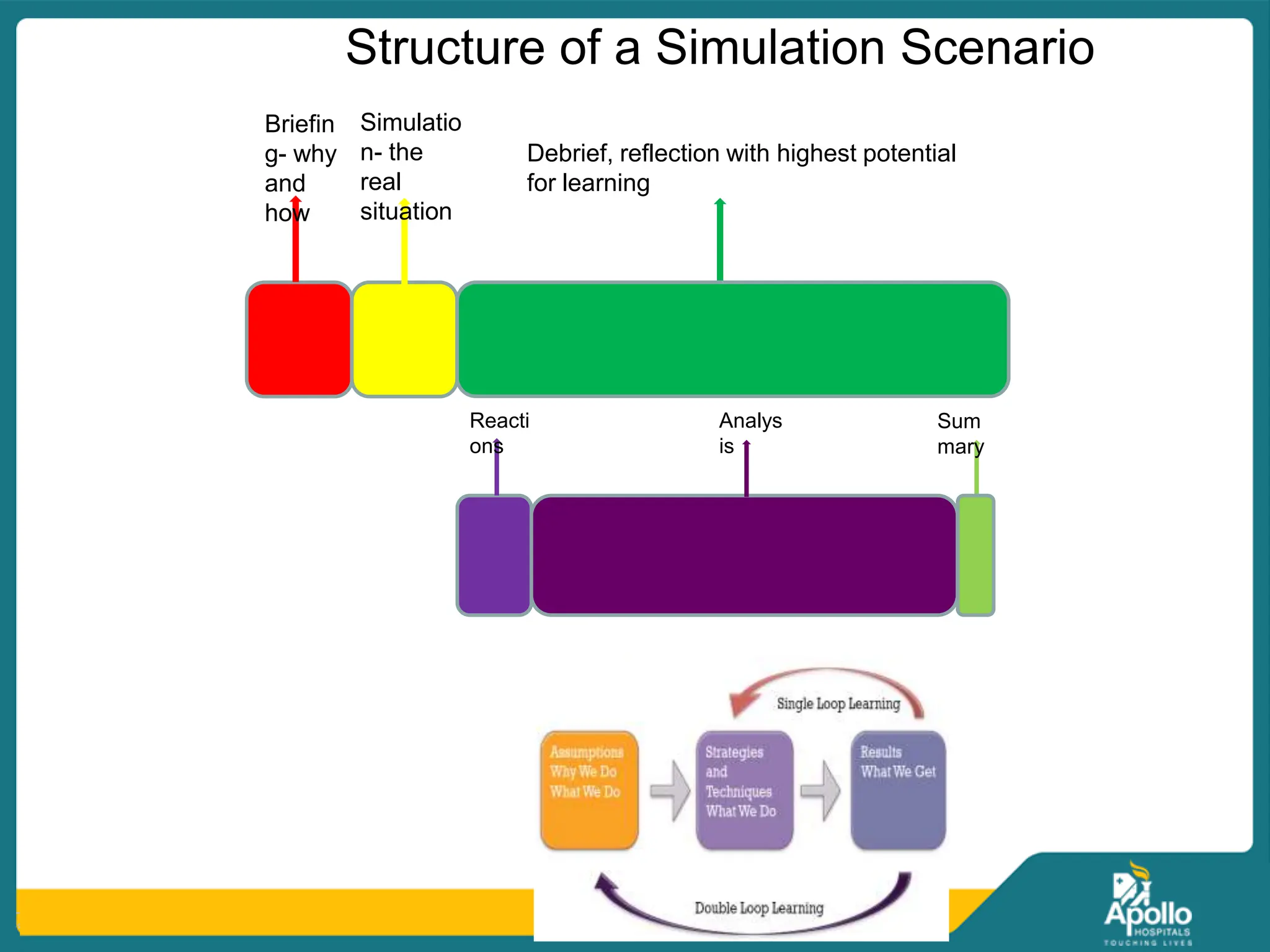
The document discusses simulation-based learning in healthcare, highlighting its definition, importance, historical development, and types. It emphasizes the benefits of creating a safe environment for skill practice and addresses the effective use of resources, assessment, and debriefing strategies. Simulation is portrayed as a crucial educational tool that improves clinician competence and patient safety through repeated practice and reflective learning.