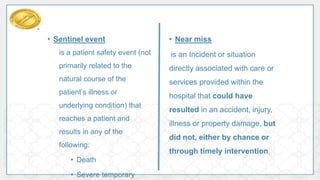
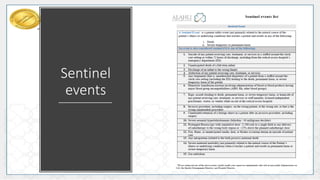
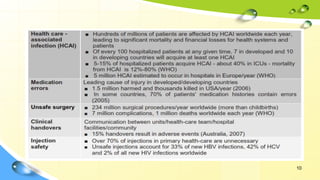
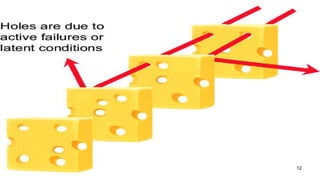
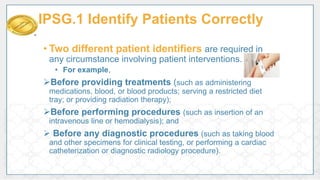
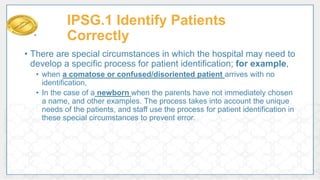
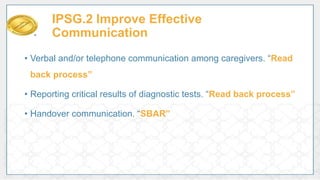
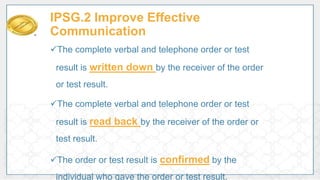
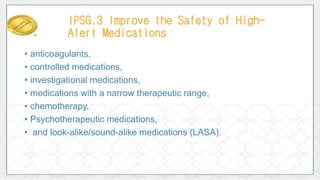
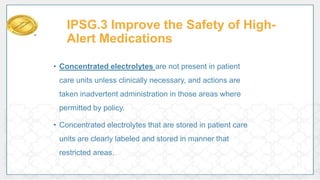
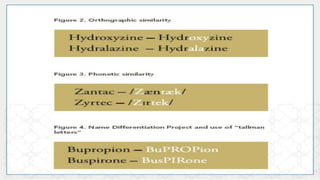
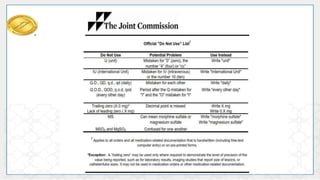
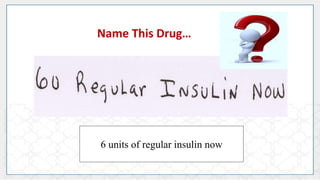
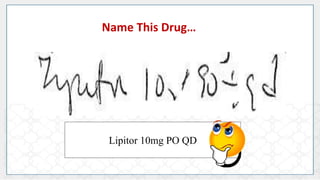
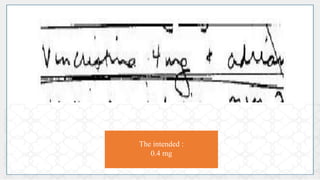
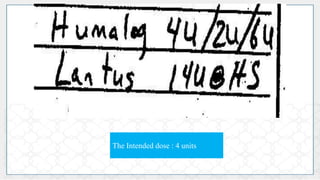
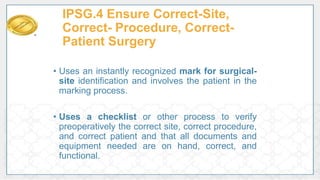
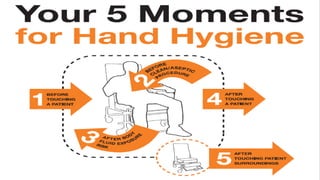
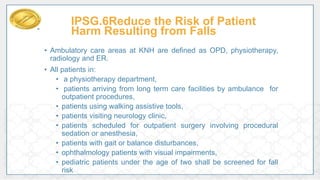
This document discusses patient safety and the International Patient Safety Goals. It defines patient safety as the prevention of errors and adverse effects associated with healthcare. It also defines key terms like sentinel events and near misses. The document then summarizes each of the 6 International Patient Safety Goals which focus on correctly identifying patients, improving communication, safety of high-alert medications, correct site surgery, reducing healthcare associated infections, and reducing falls. It provides examples of processes to meet each goal.