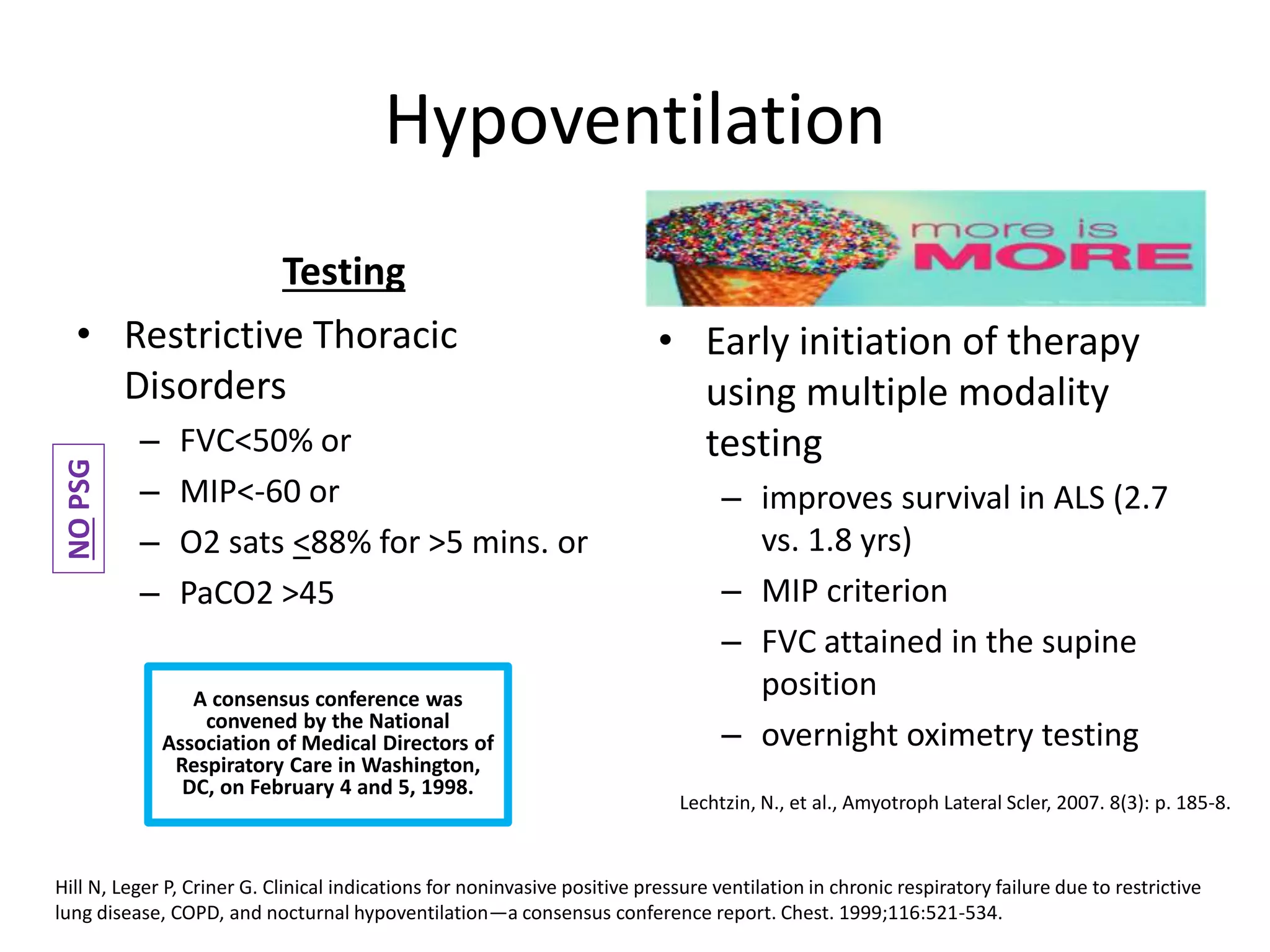
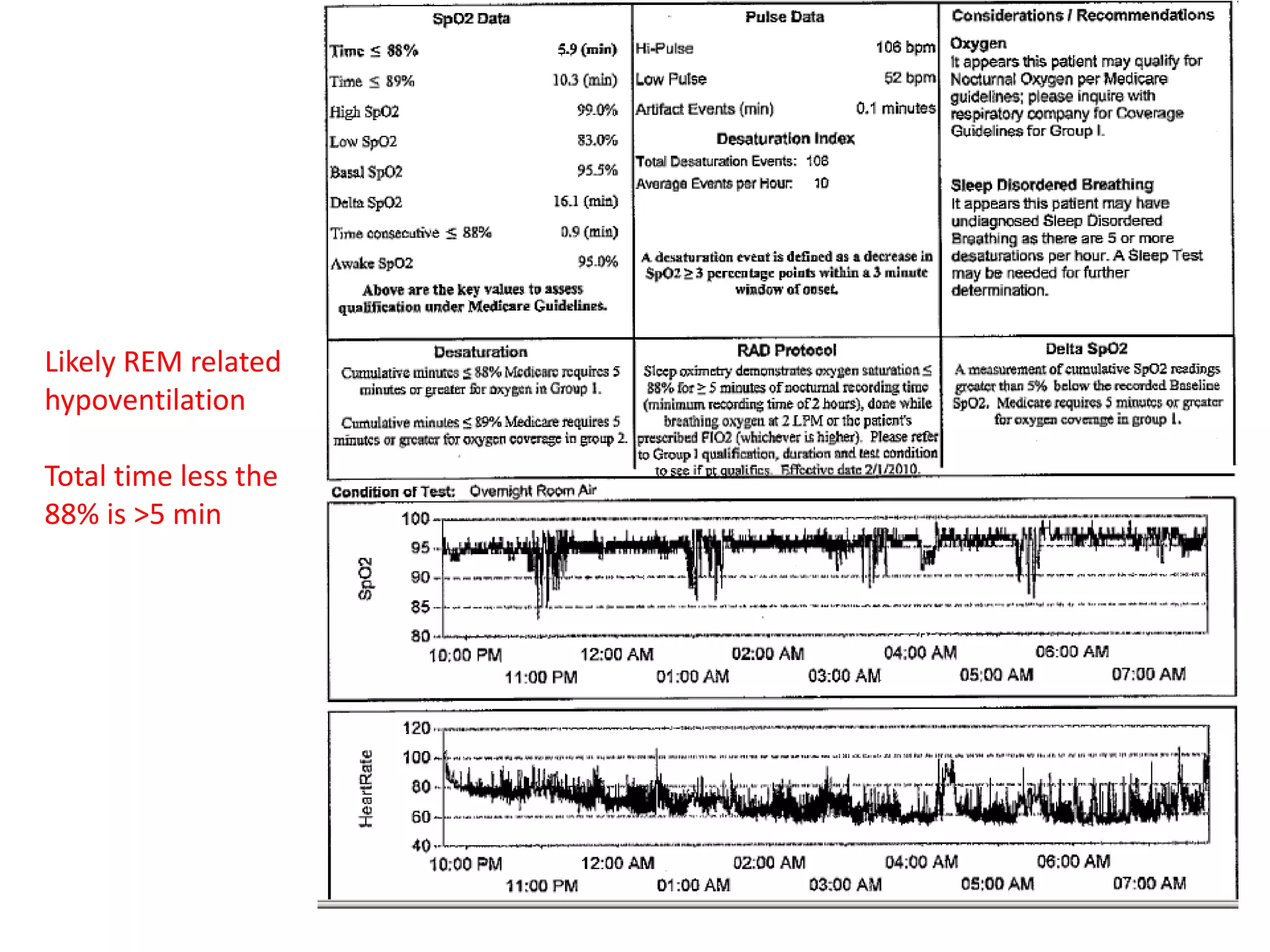
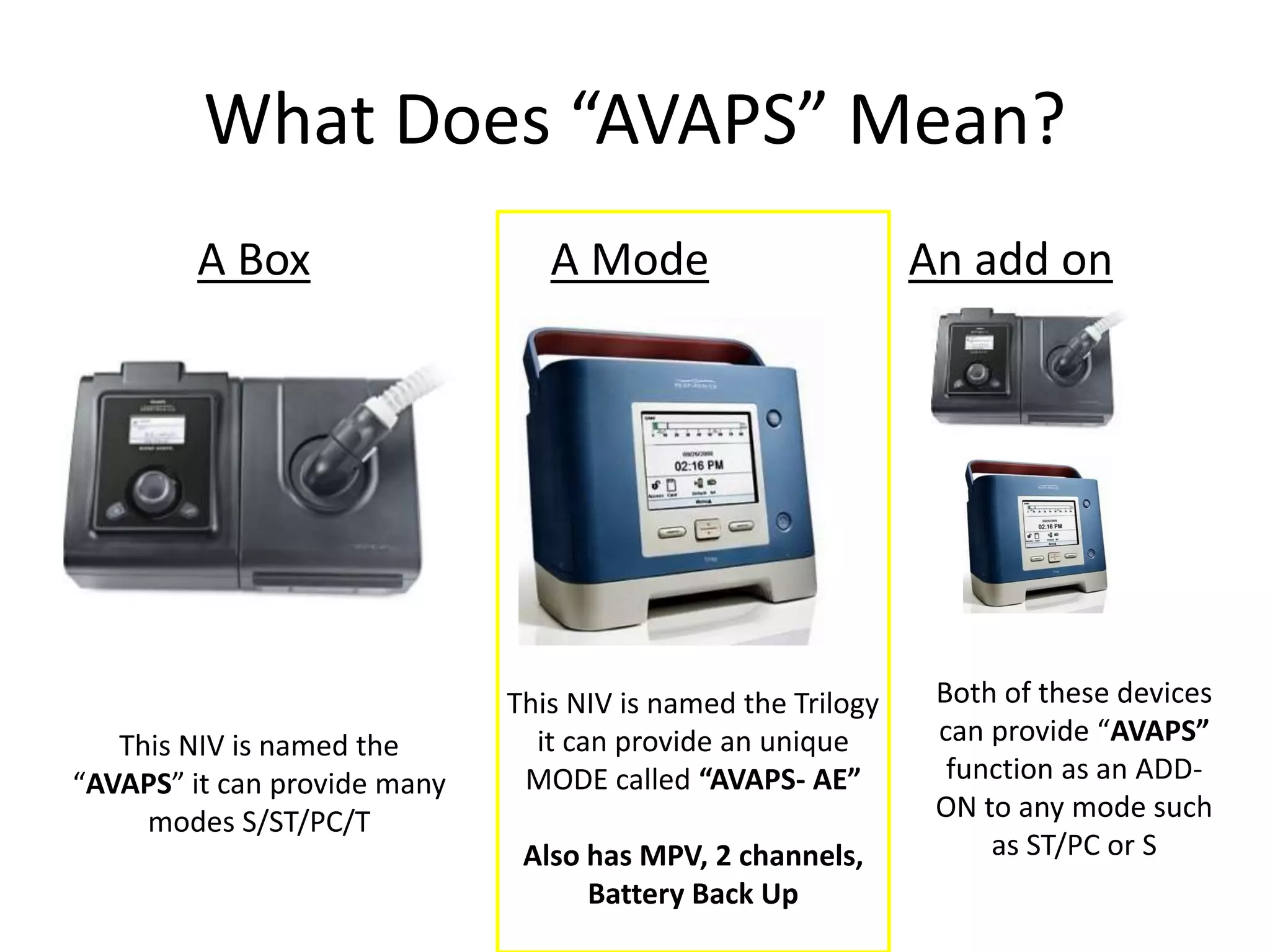
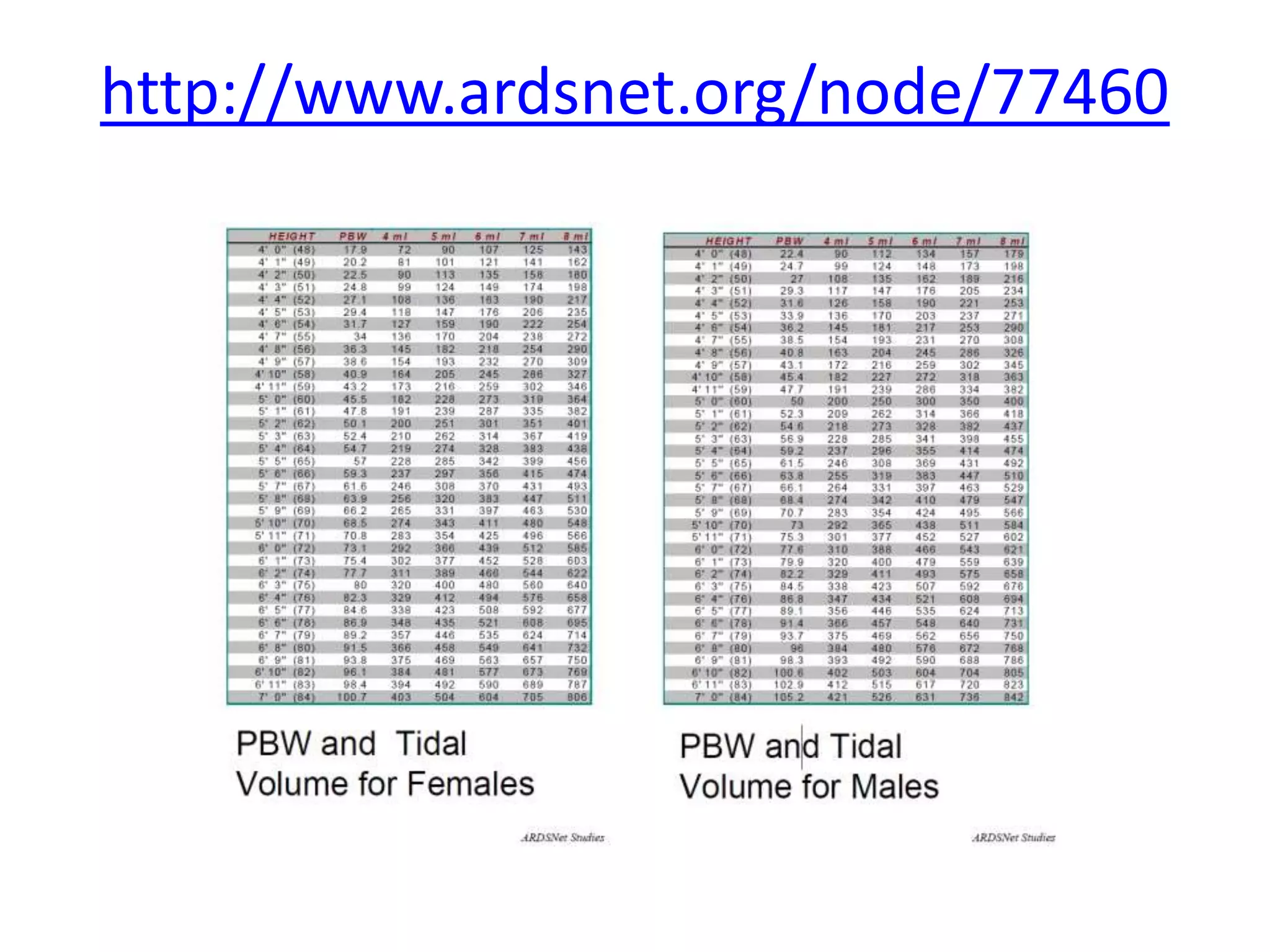
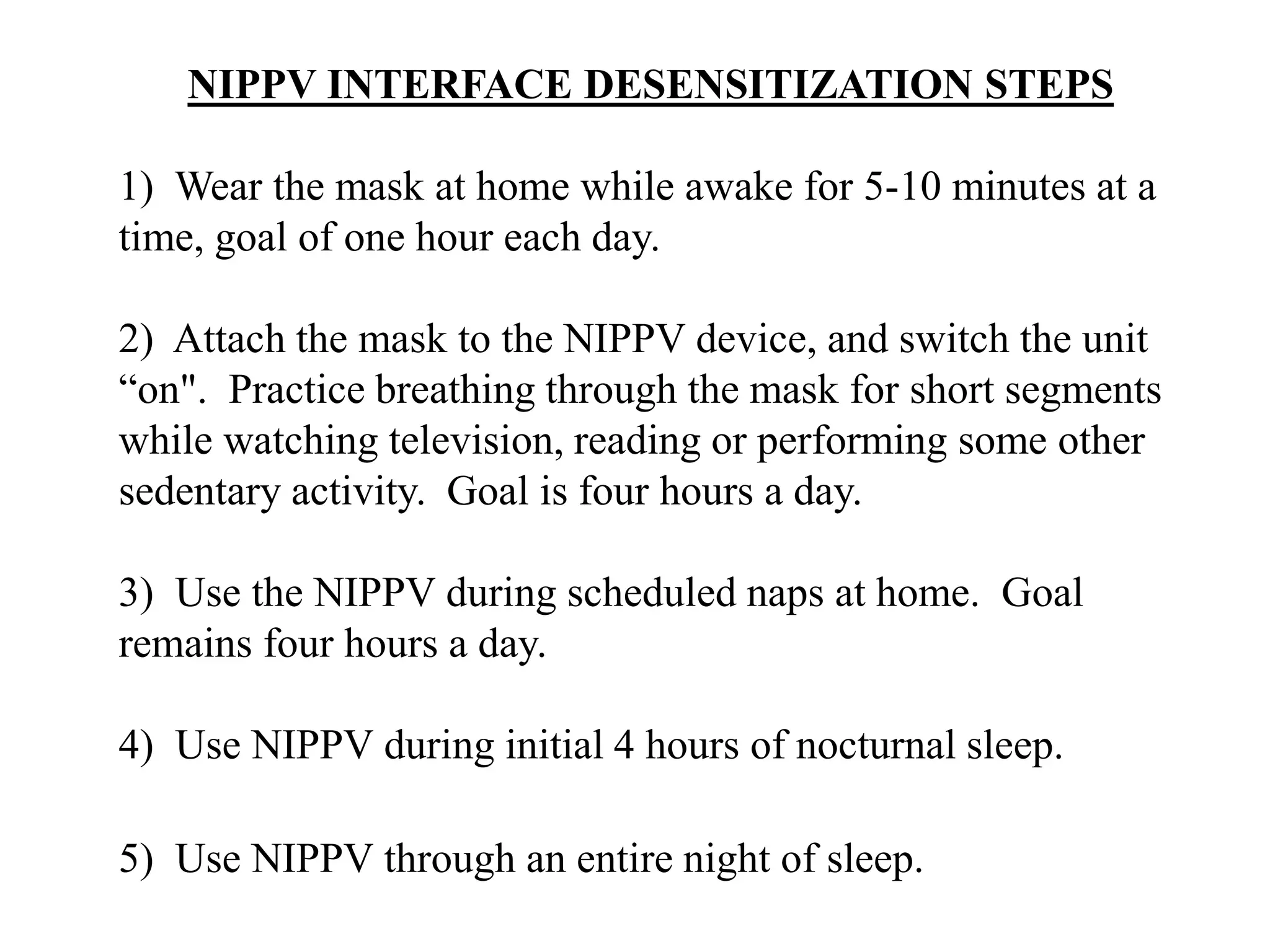
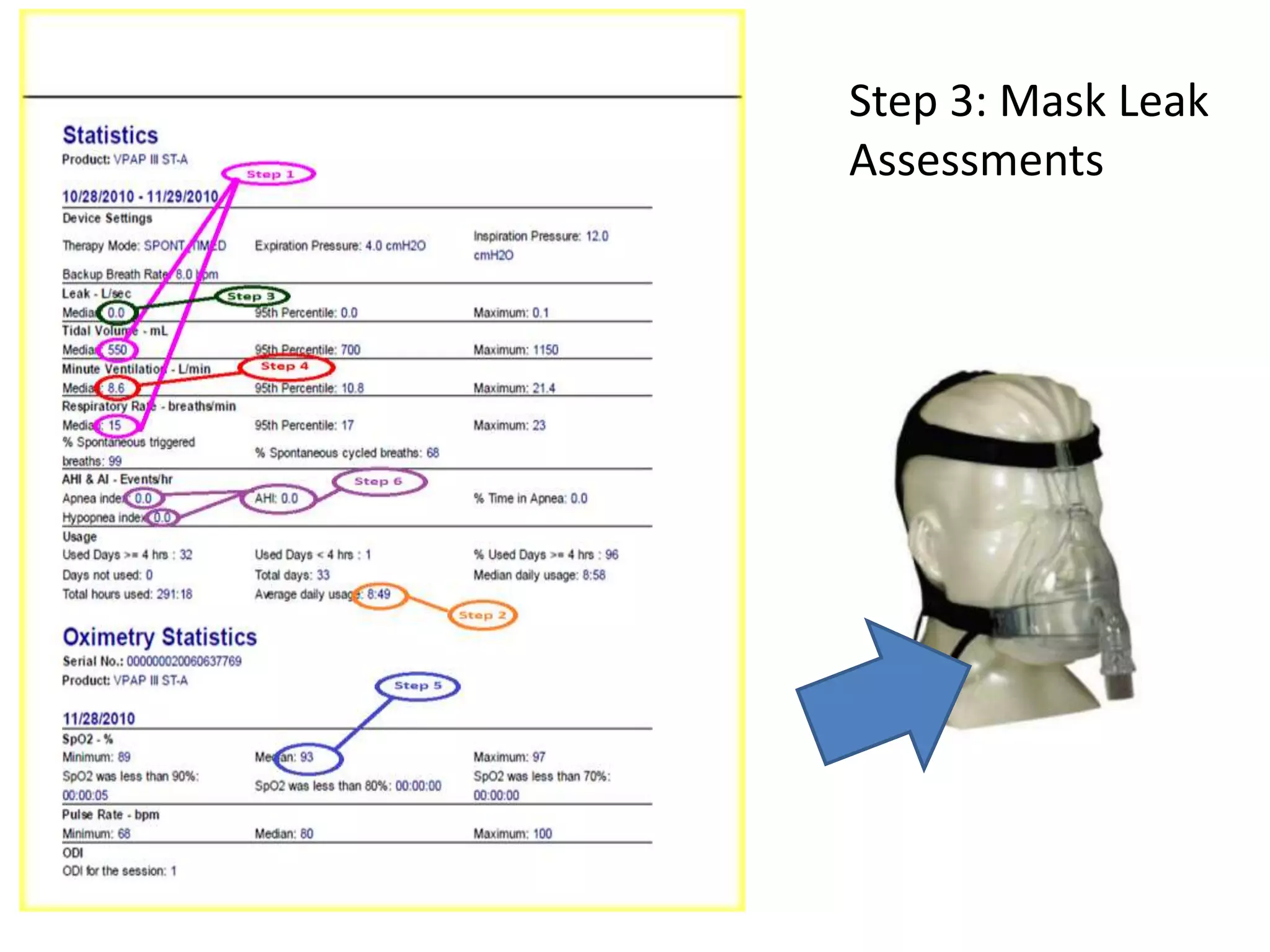
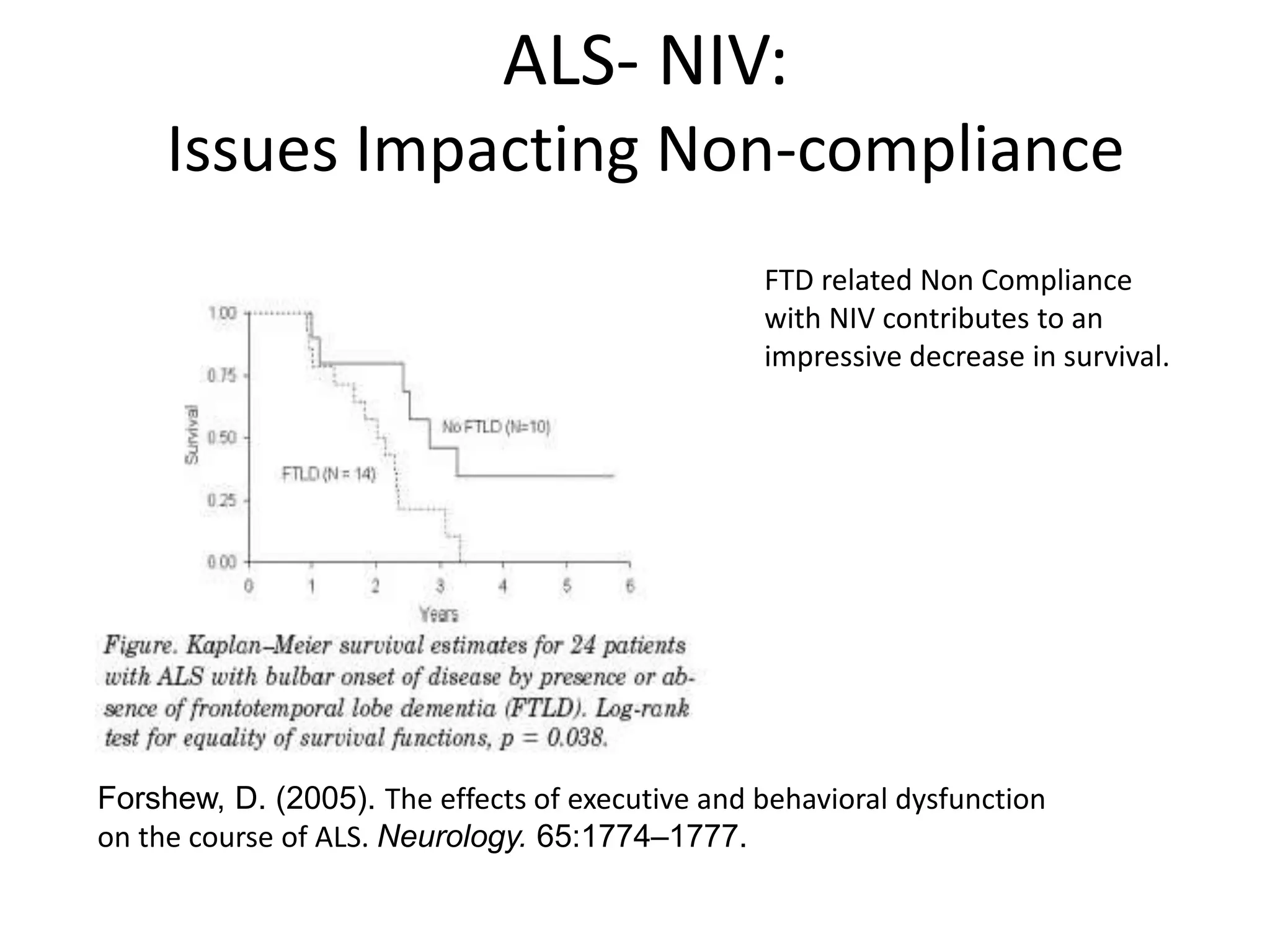
This document provides an overview of optimizing respiratory care for patients with ALS. It discusses testing and treatment for hypoventilation including non-invasive ventilation. It reviews various modes, settings, and features of non-invasive ventilators. It also covers monitoring downloads, interfaces, desensitization steps, and assessing tidal volume, usage, leaks, minute ventilation, pulse oximetry, and apnea/hypopnea to optimize care. Barriers to compliance like FTD and bulbar onset are addressed. The document provides a comprehensive guide to respiratory management in ALS.