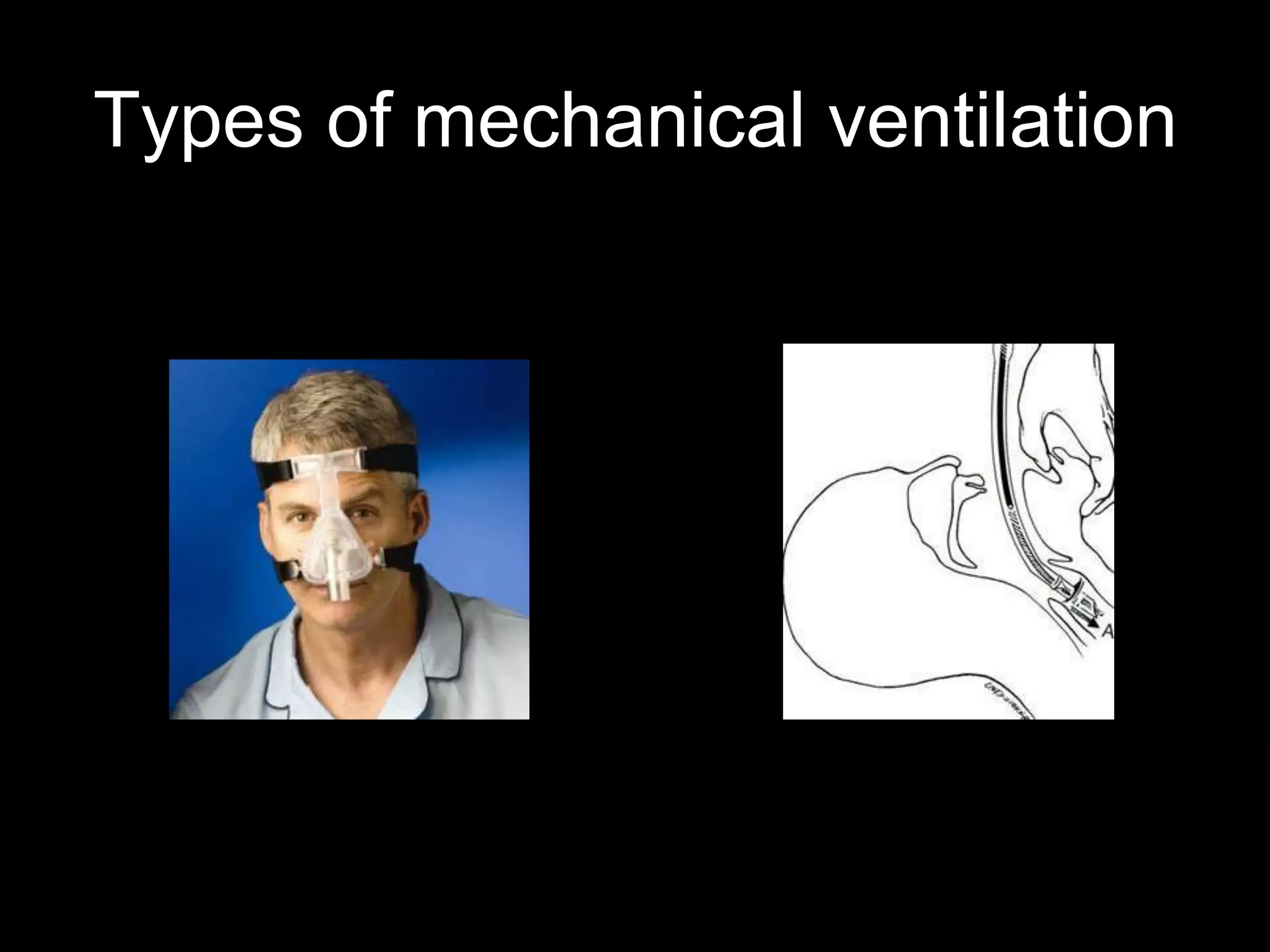
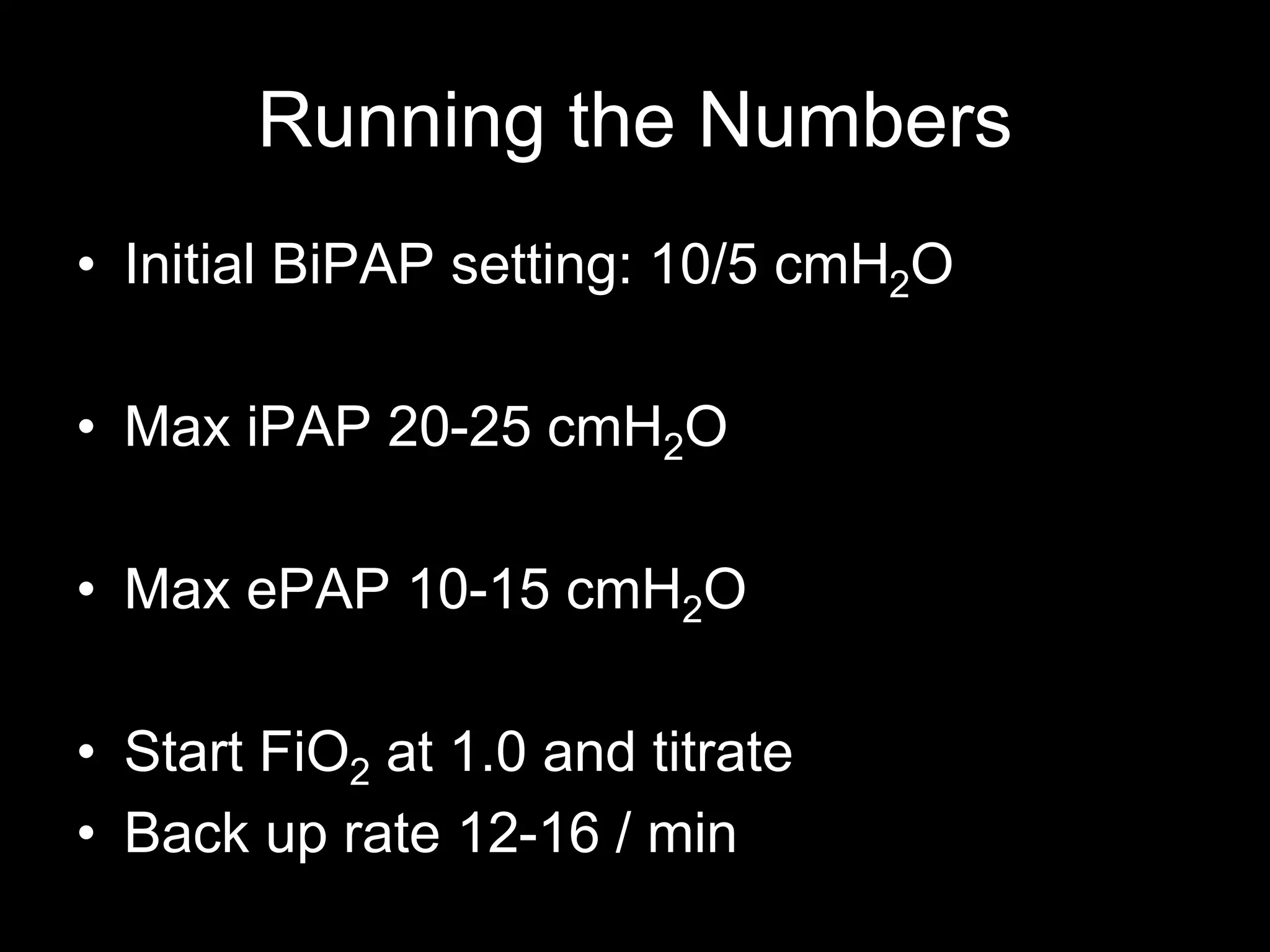
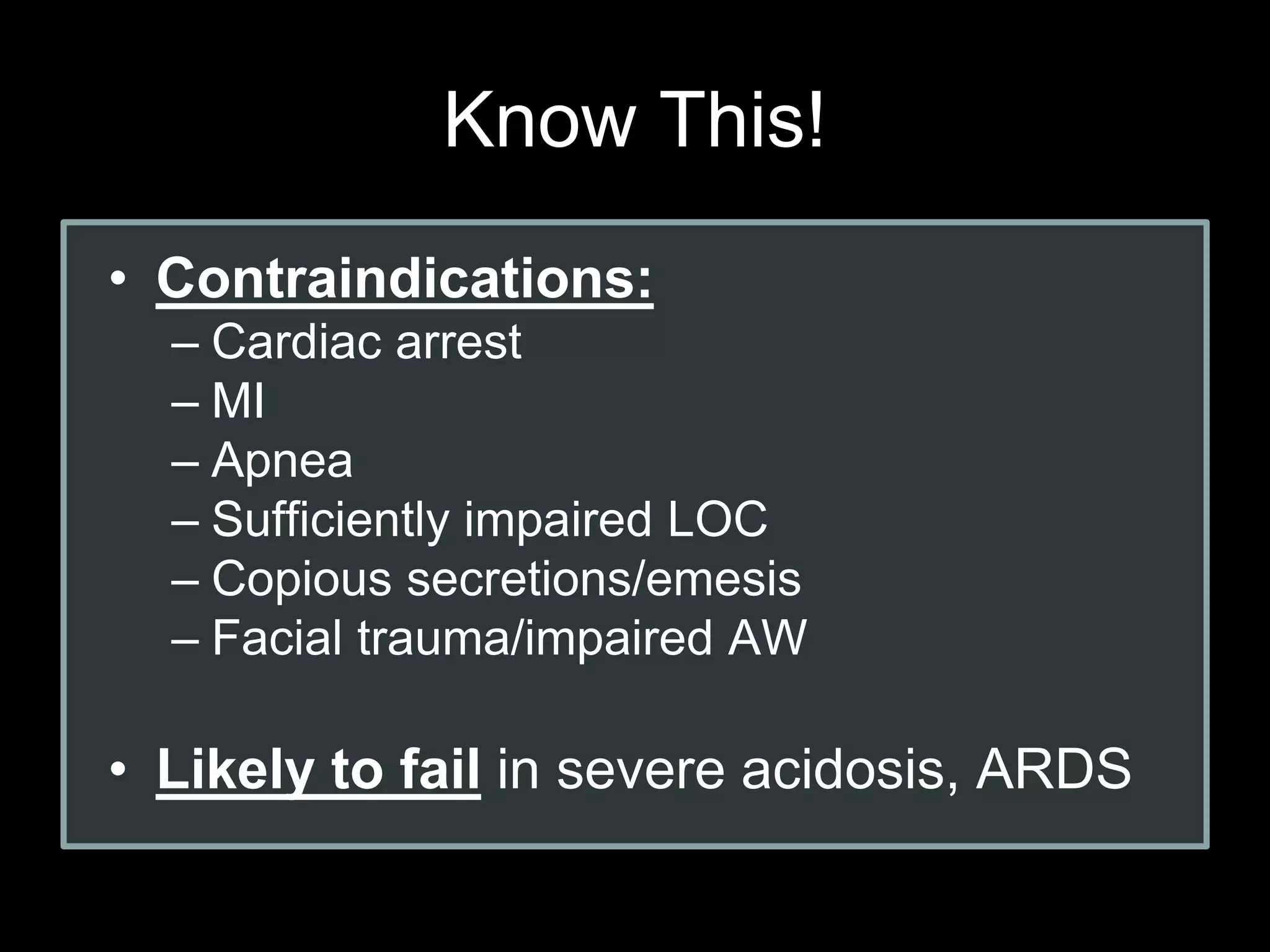
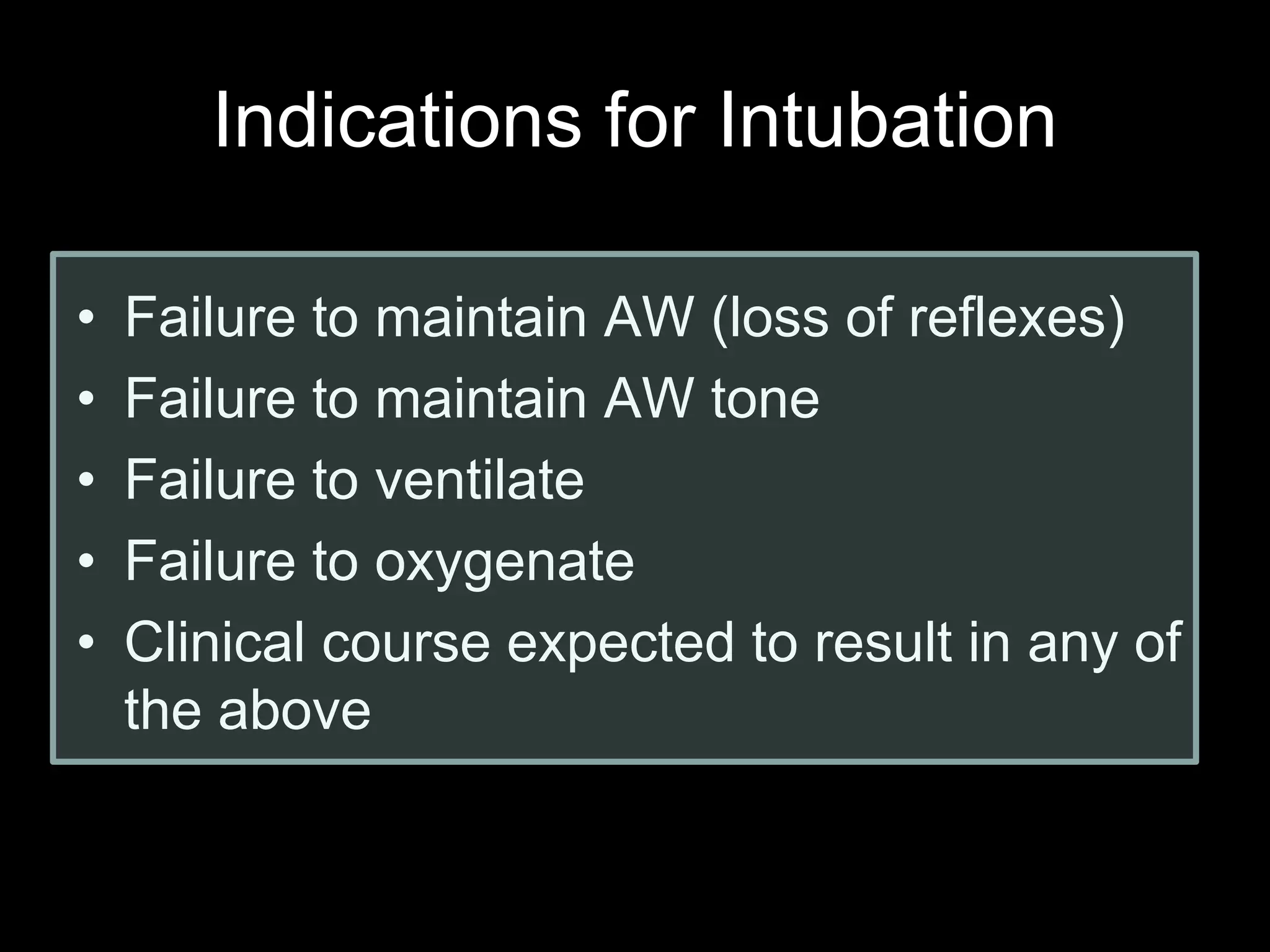
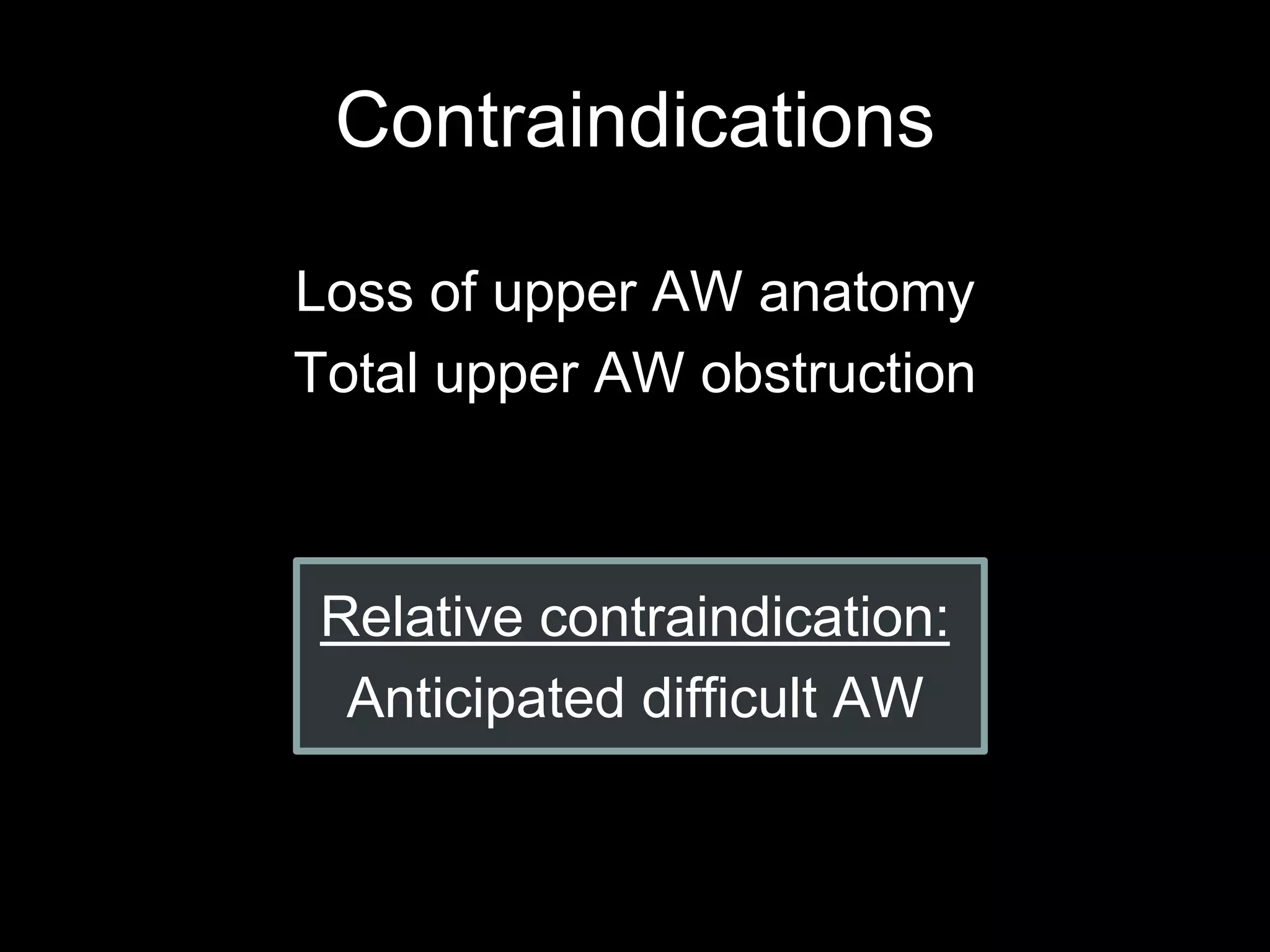
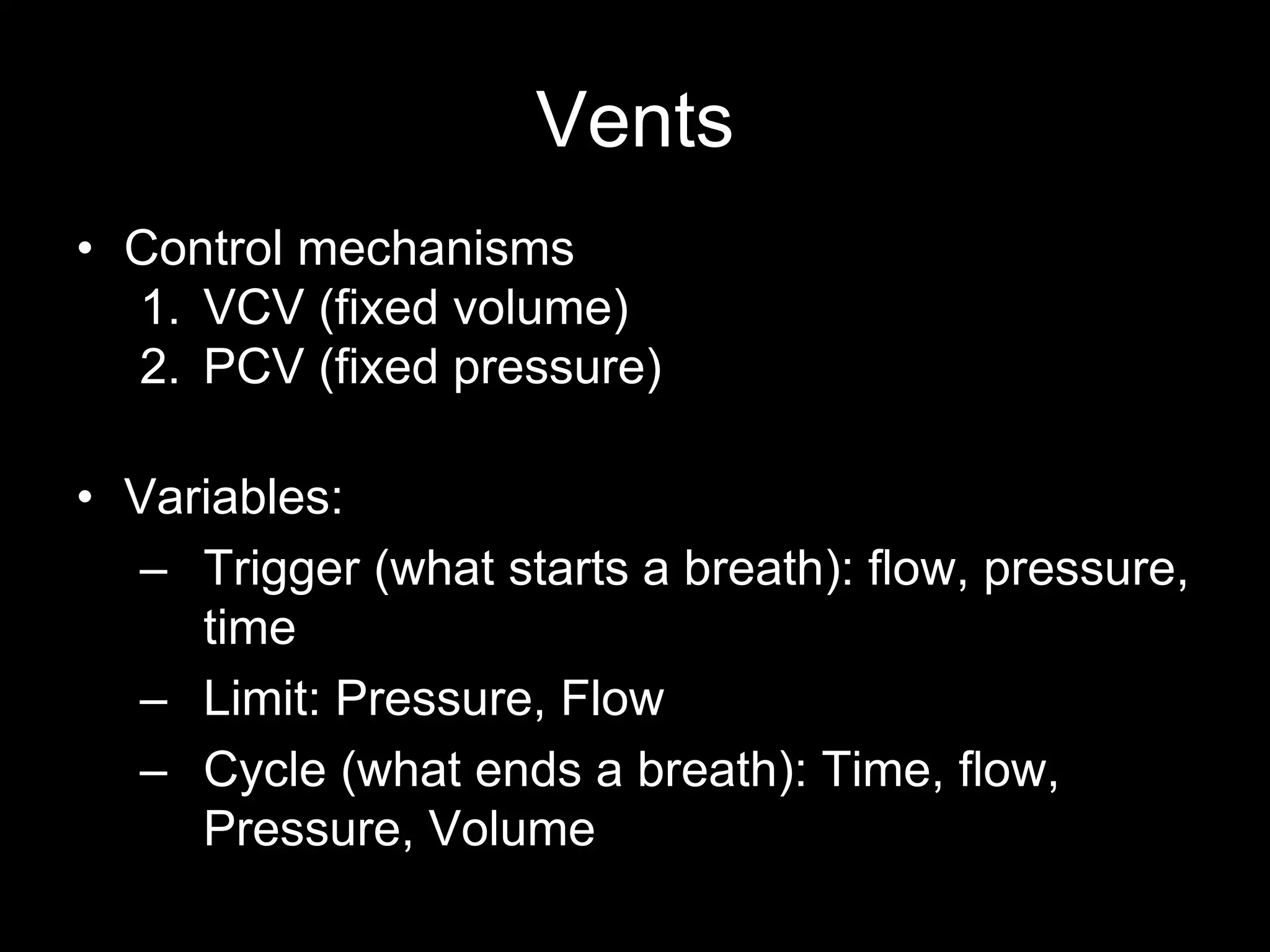
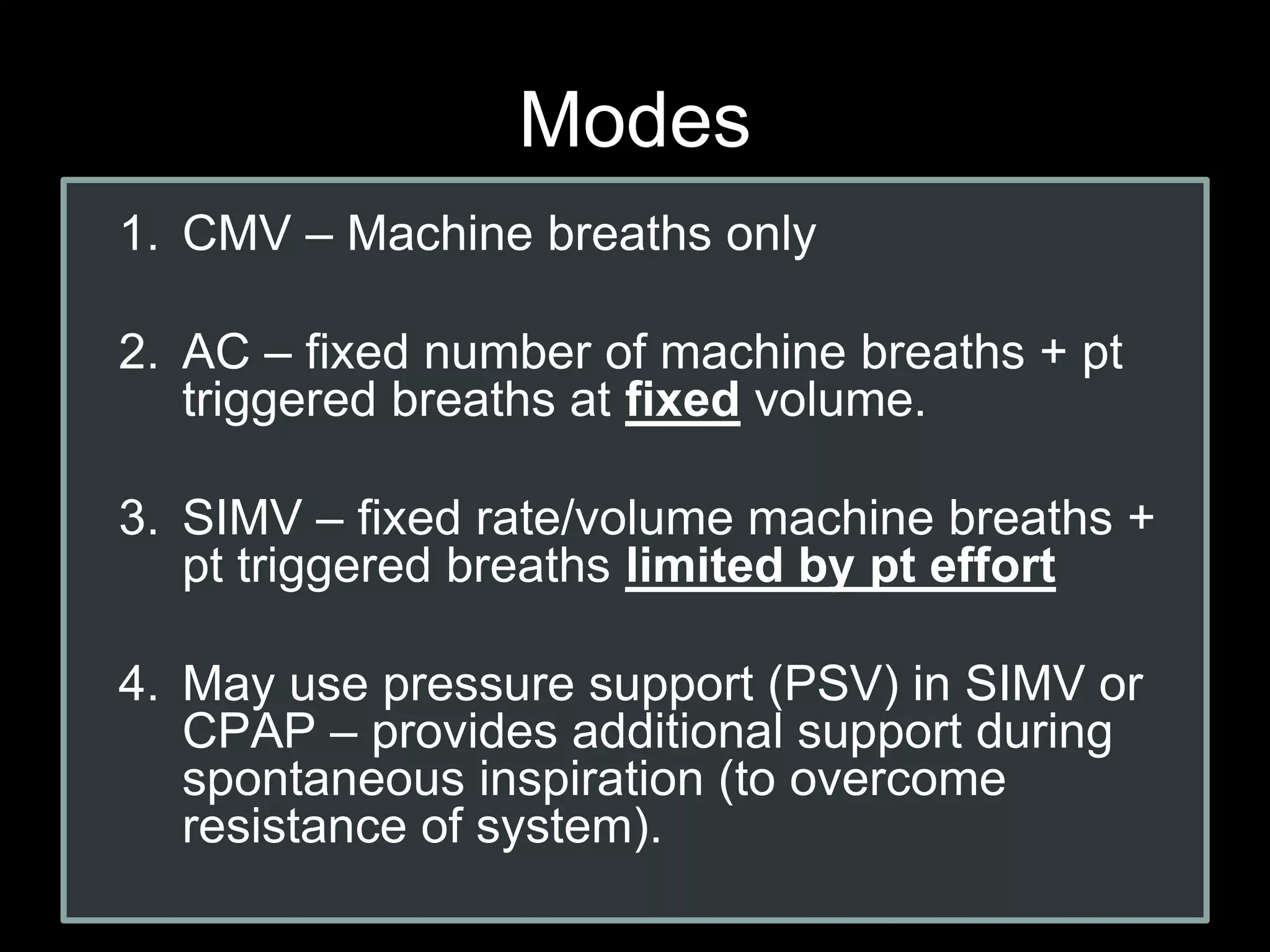
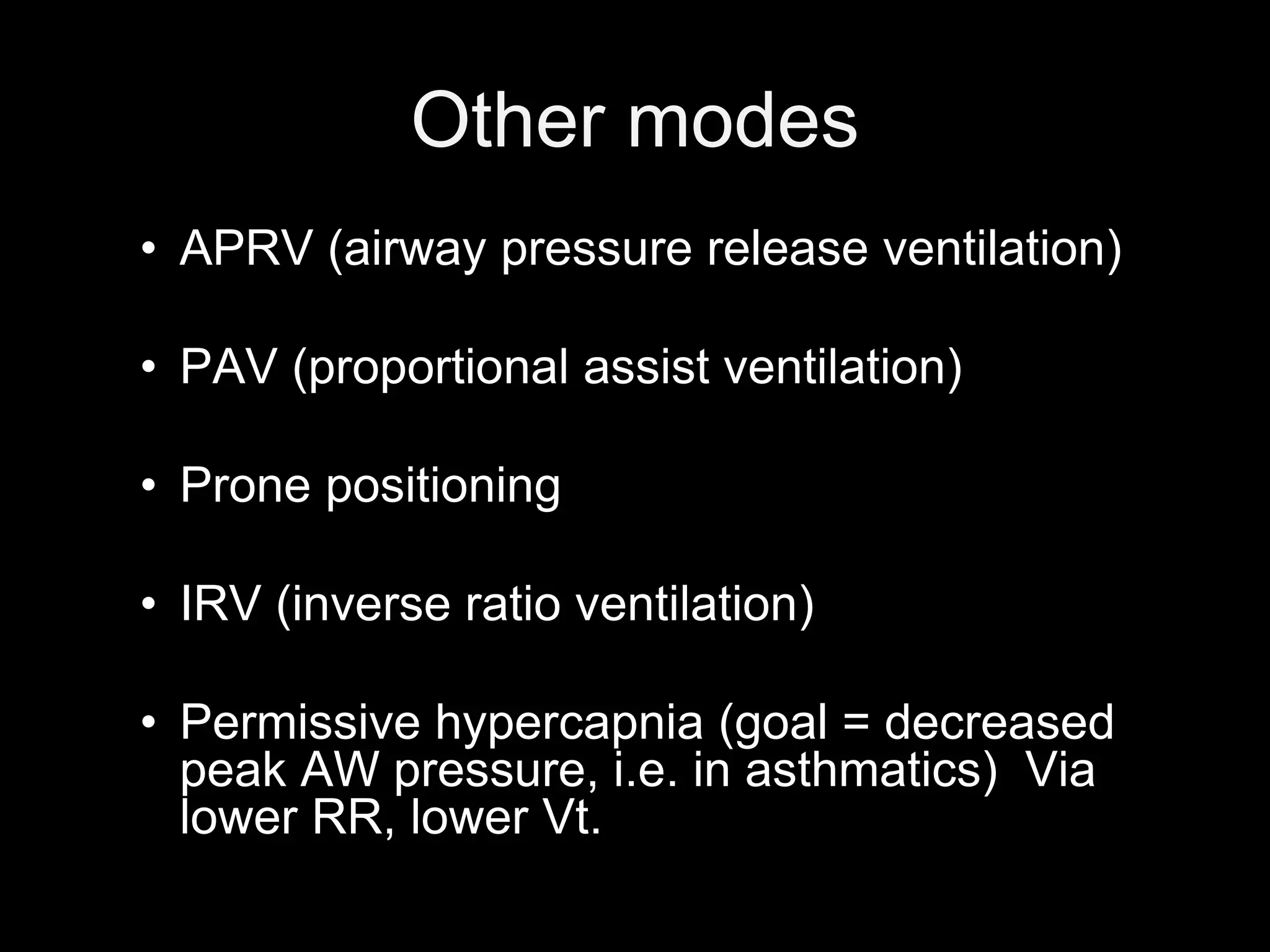
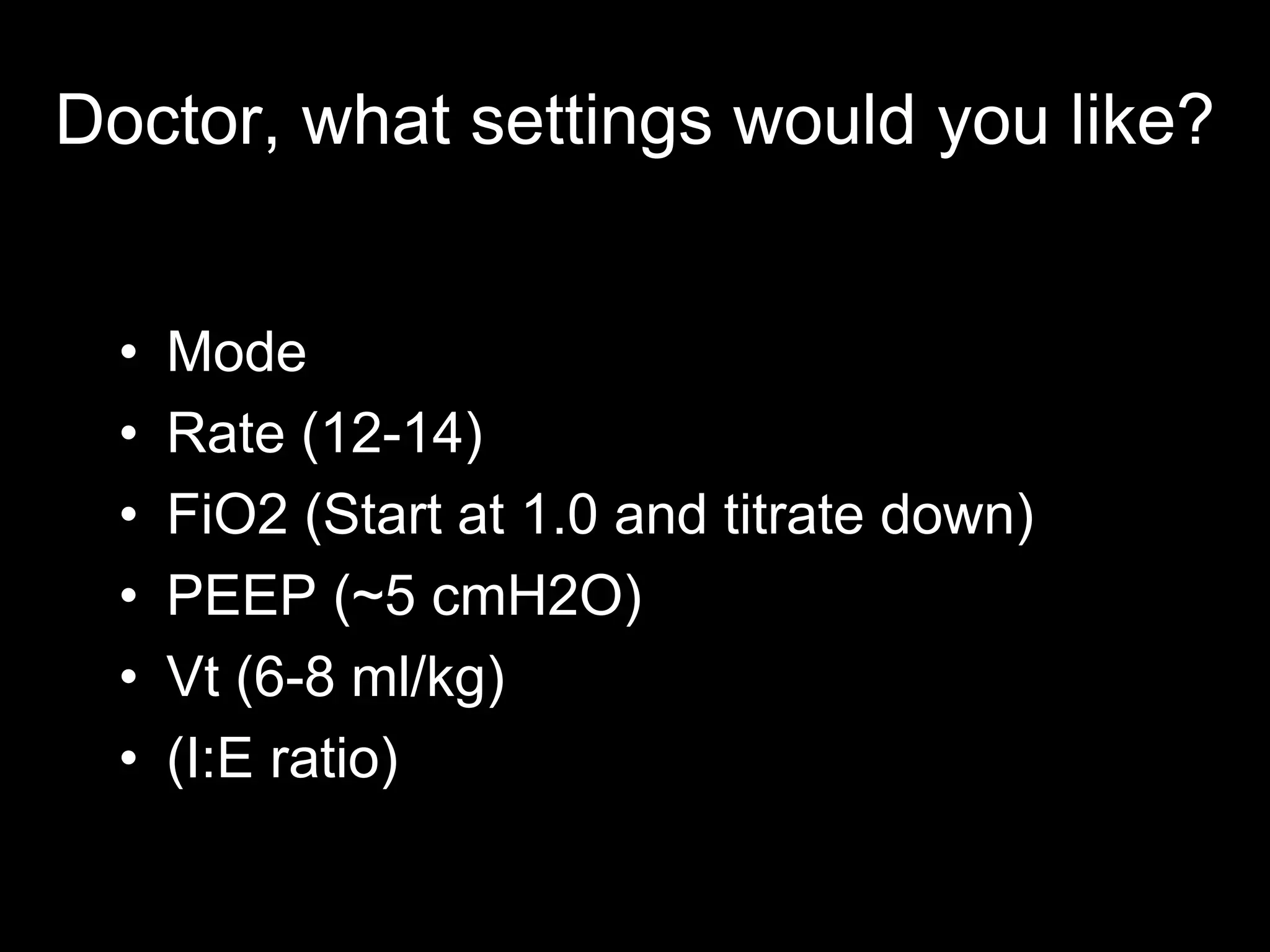
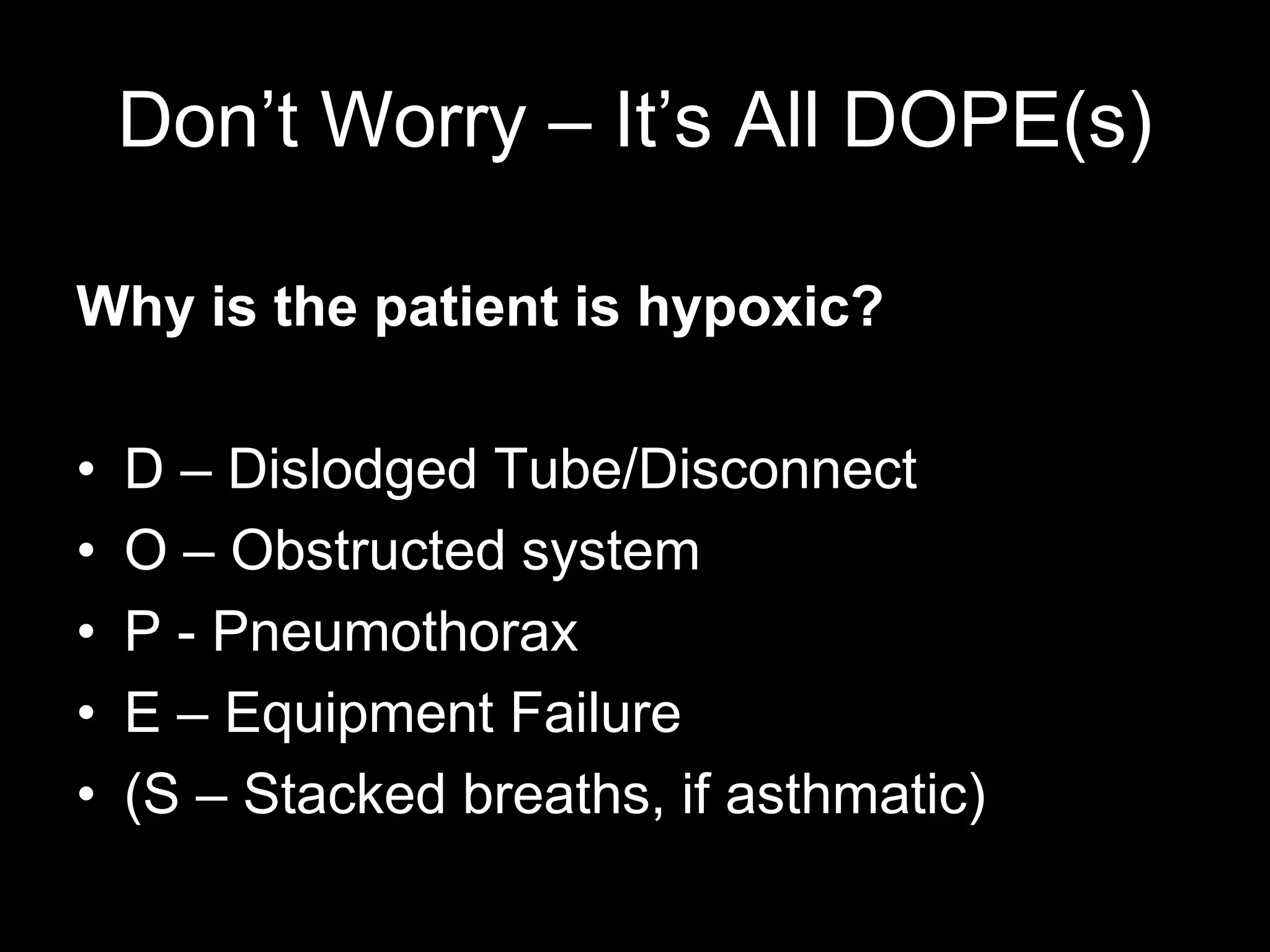
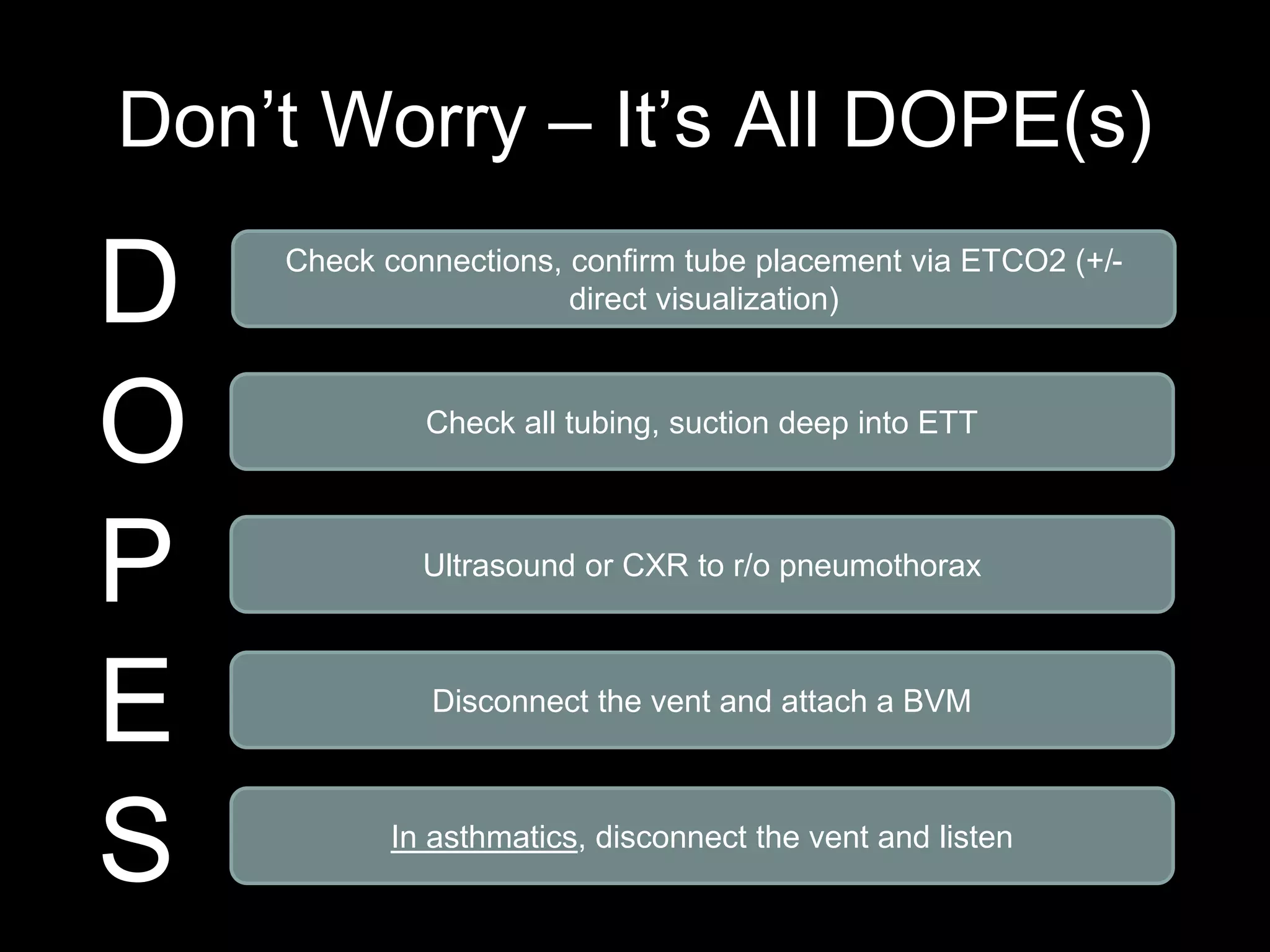
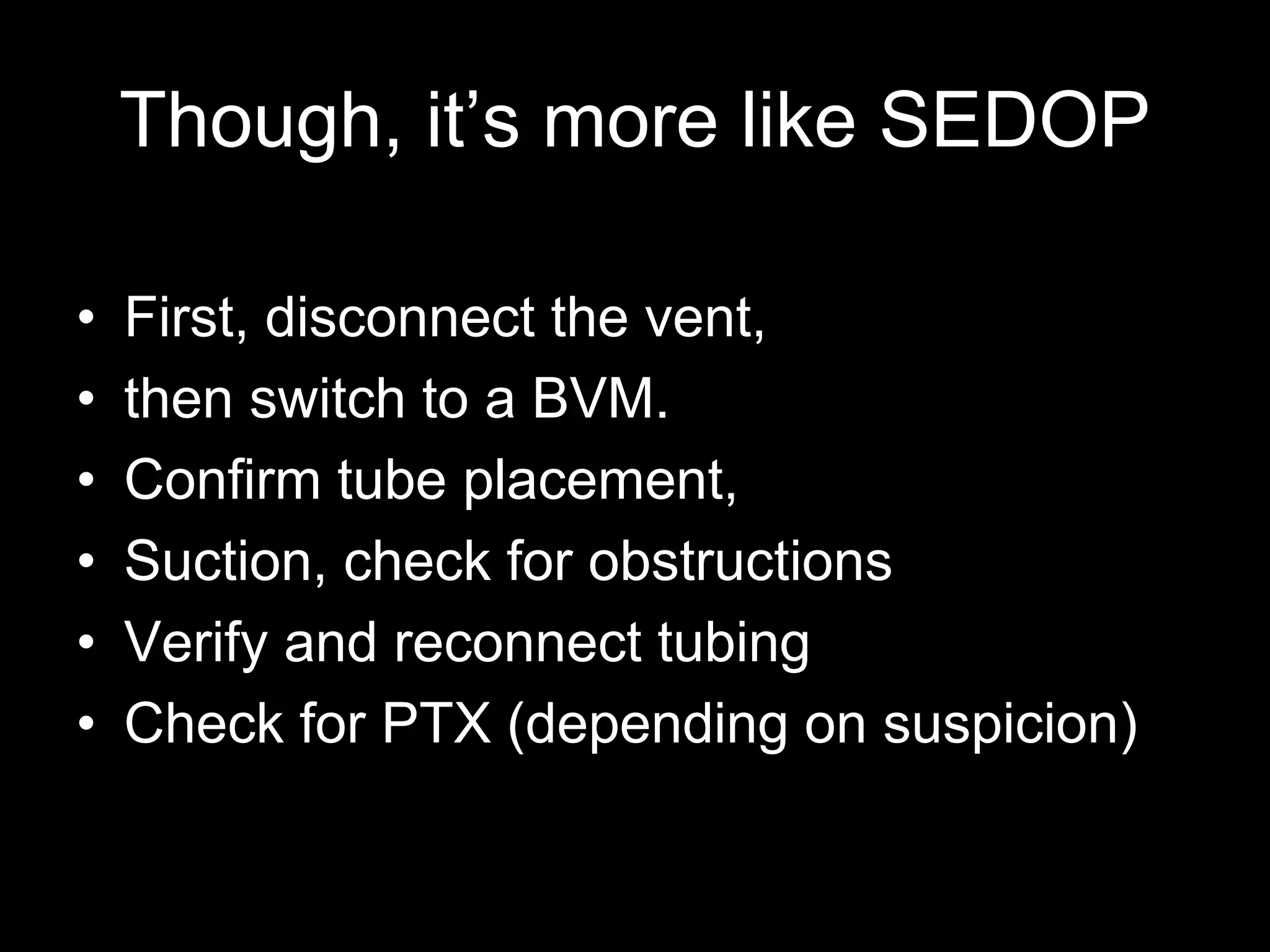
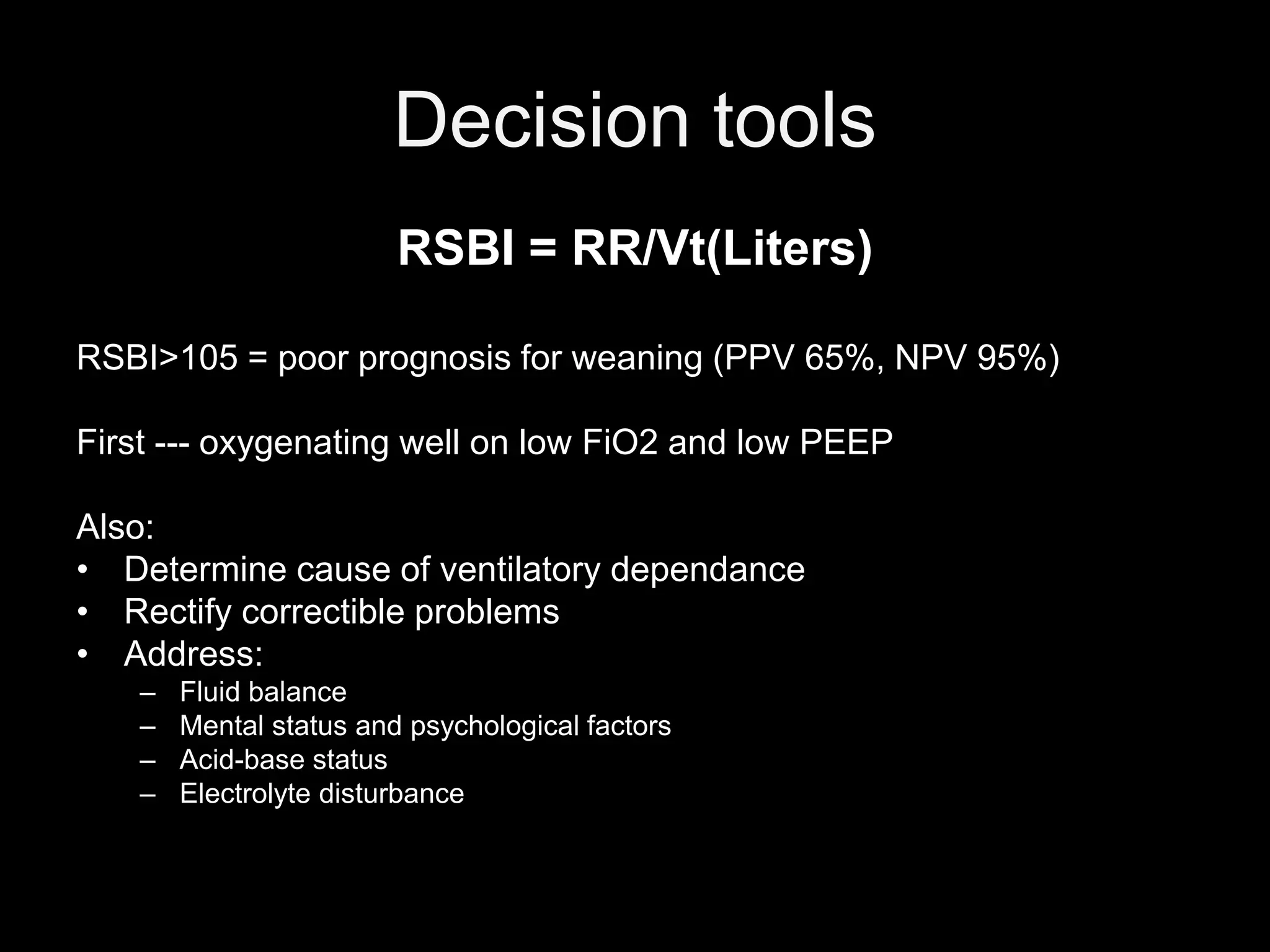
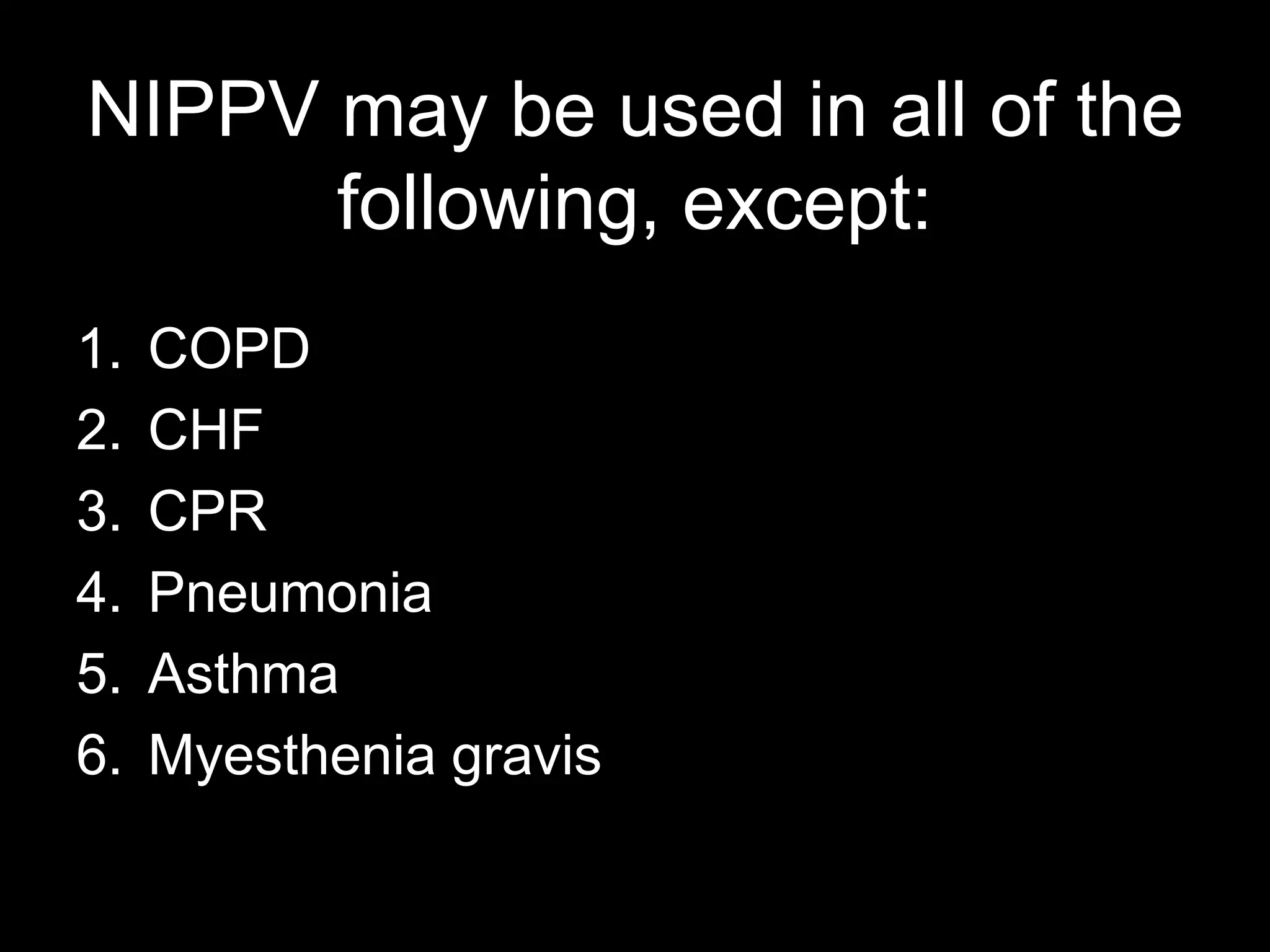
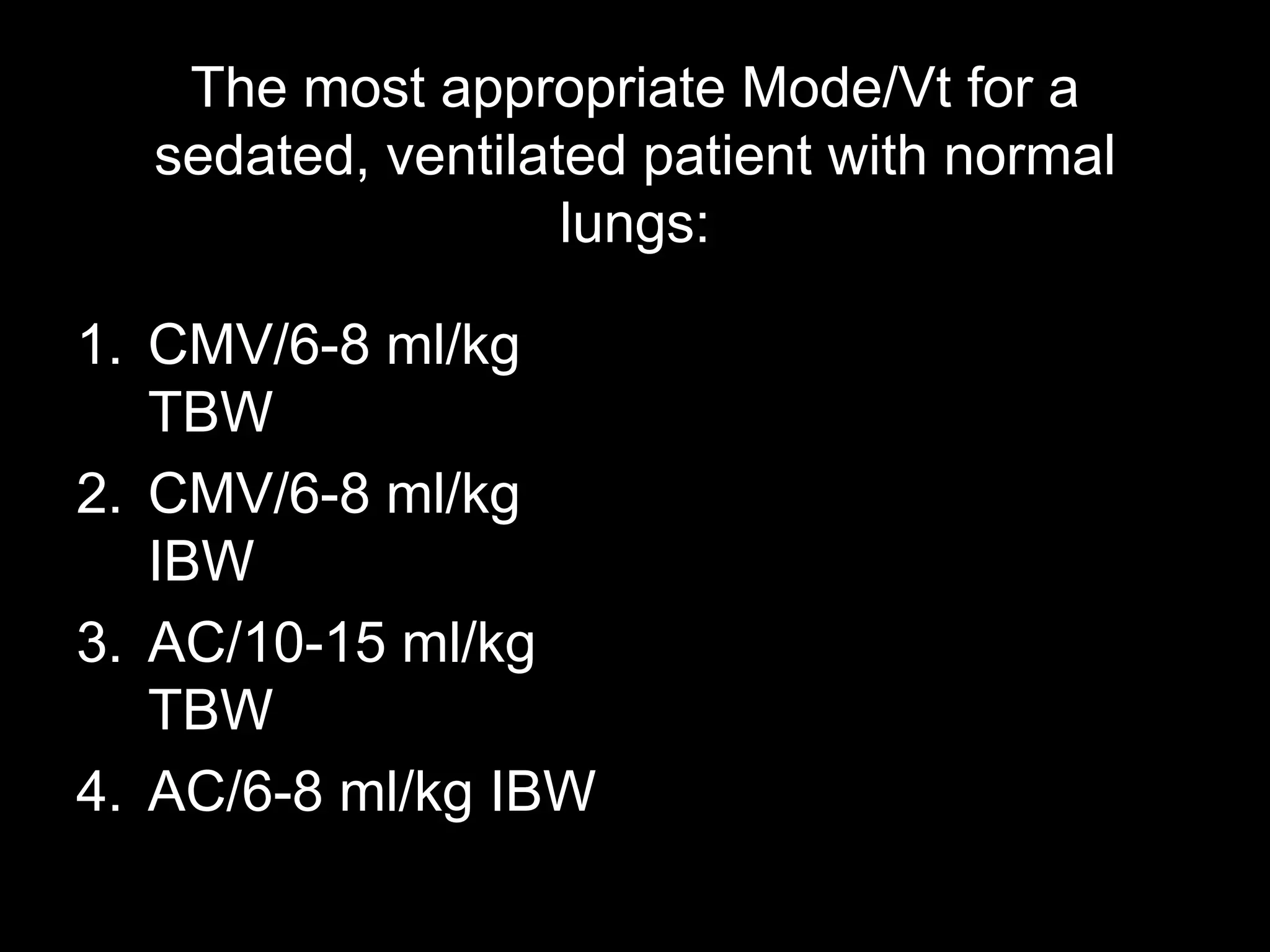
This document provides an overview of mechanical ventilation, including its goals, general principles, types, settings, monitoring, troubleshooting, indications, contraindications and complications. It discusses non-invasive positive pressure ventilation and invasive mechanical ventilation, reviewing various modes, settings, weaning methods and specific management considerations for different patient populations. The key points are monitoring patients on mechanical ventilation for oxygenation and ventilation issues, addressing those issues following the DOPE/SEDOP mnemonic, and carefully considering indications and timing for initiation and discontinuation of mechanical support.