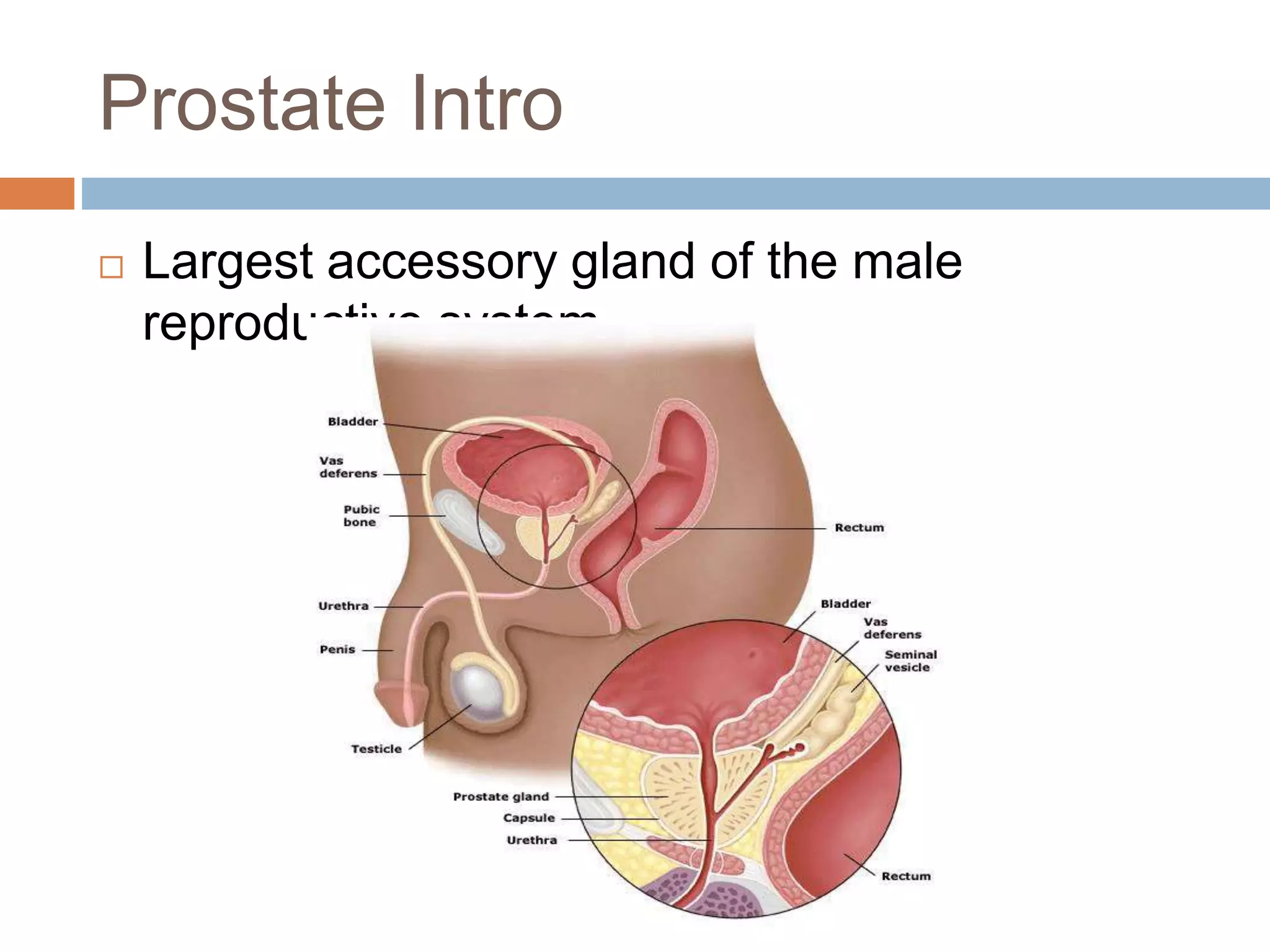
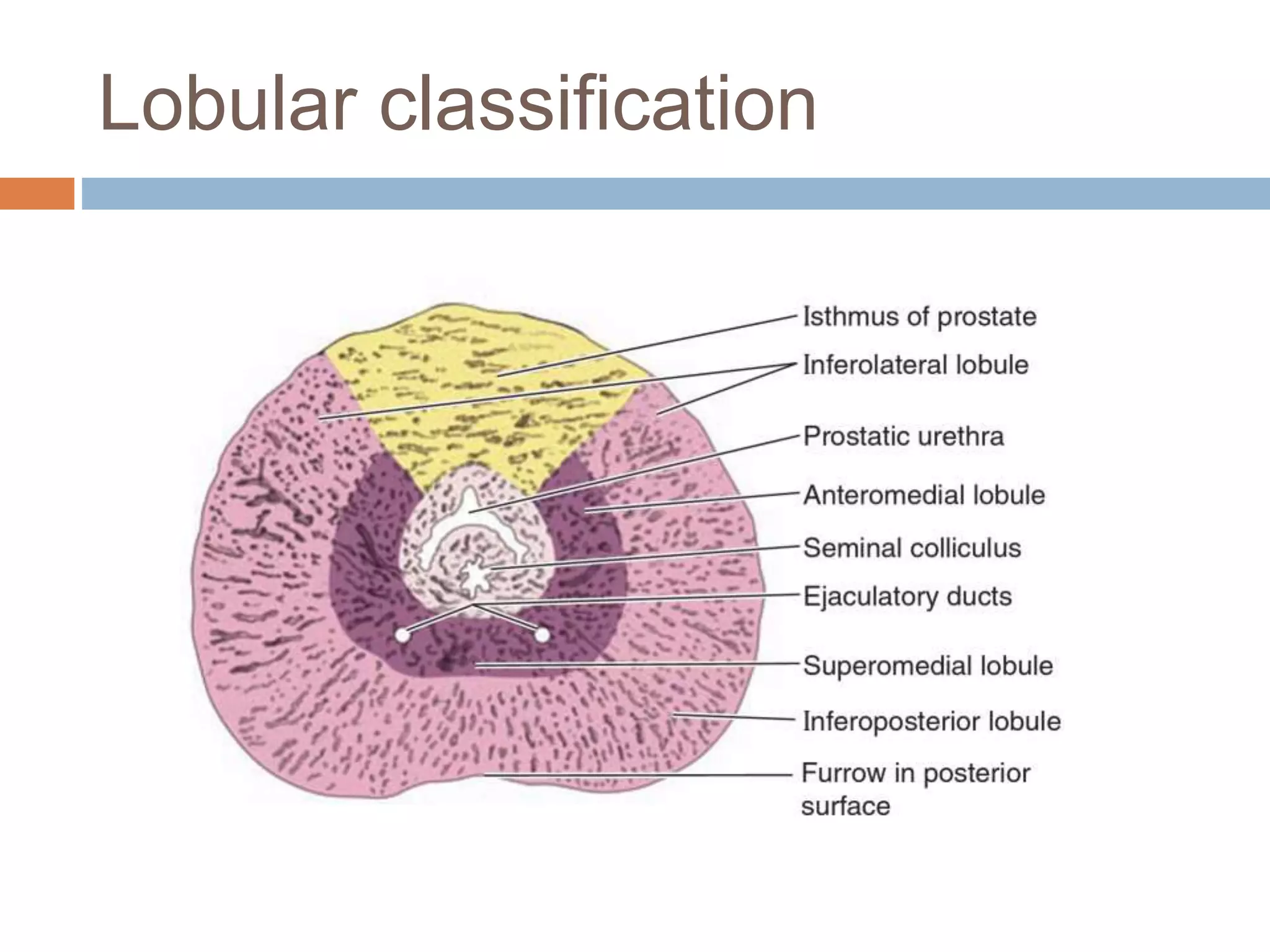
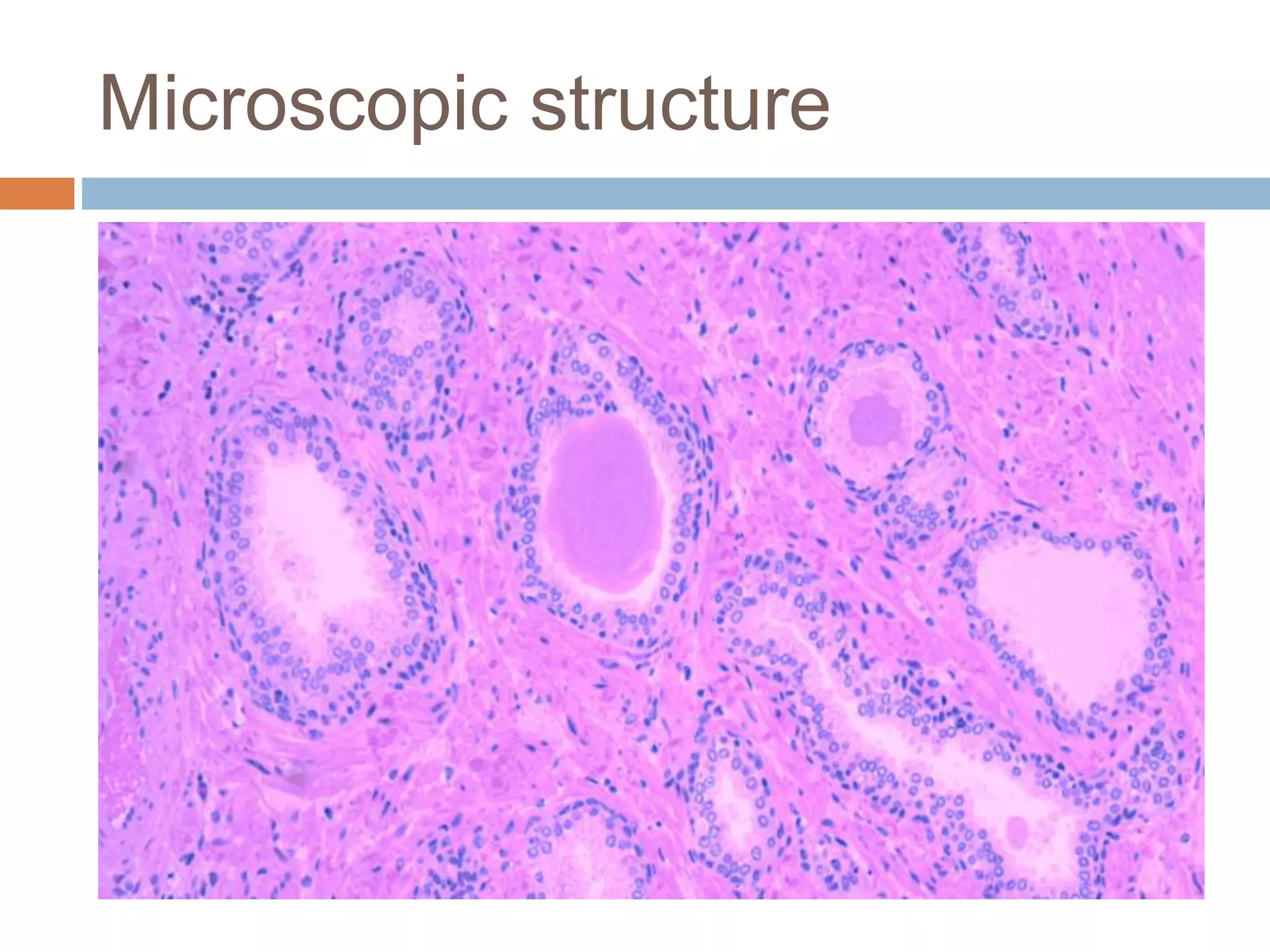
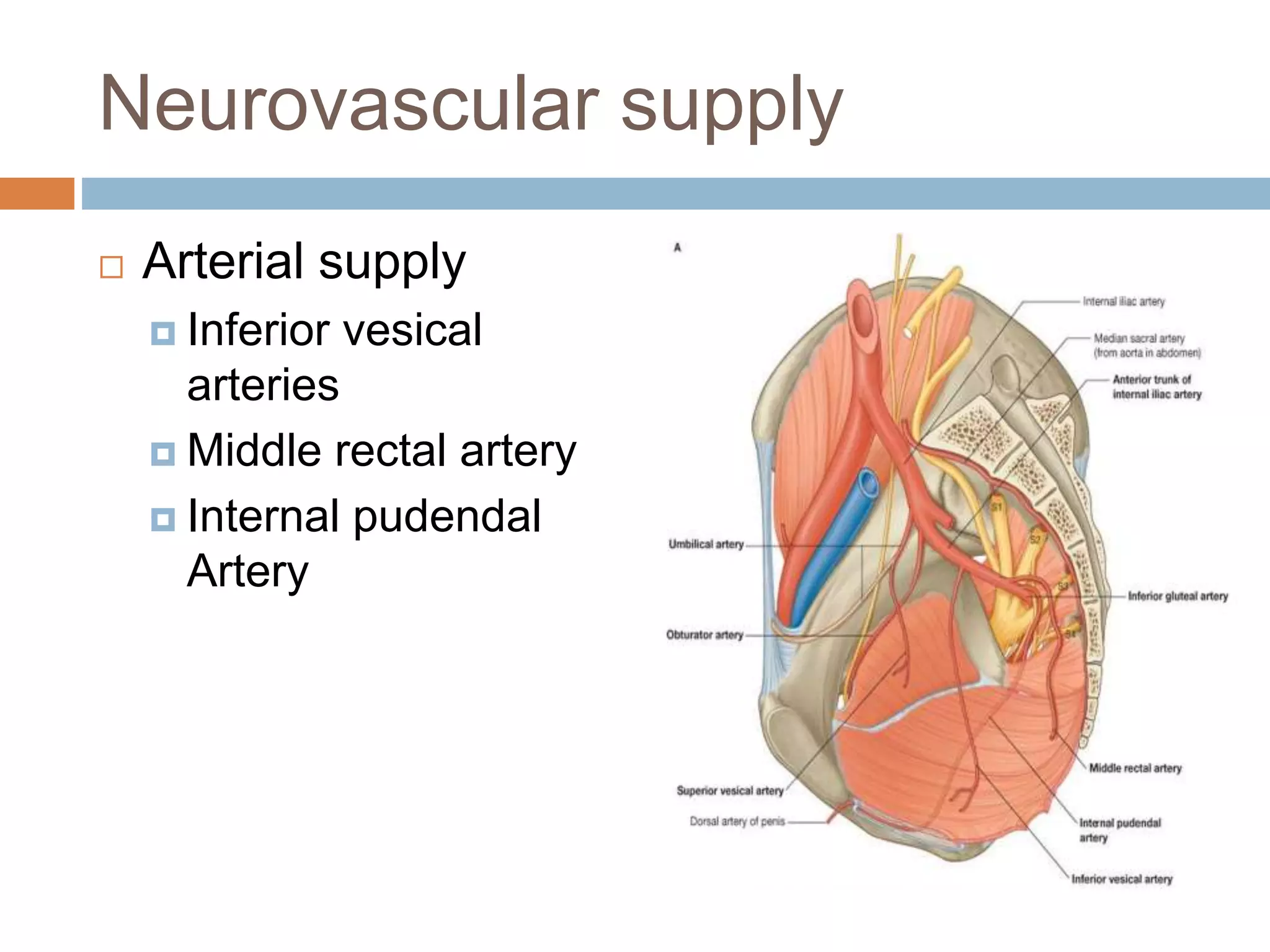
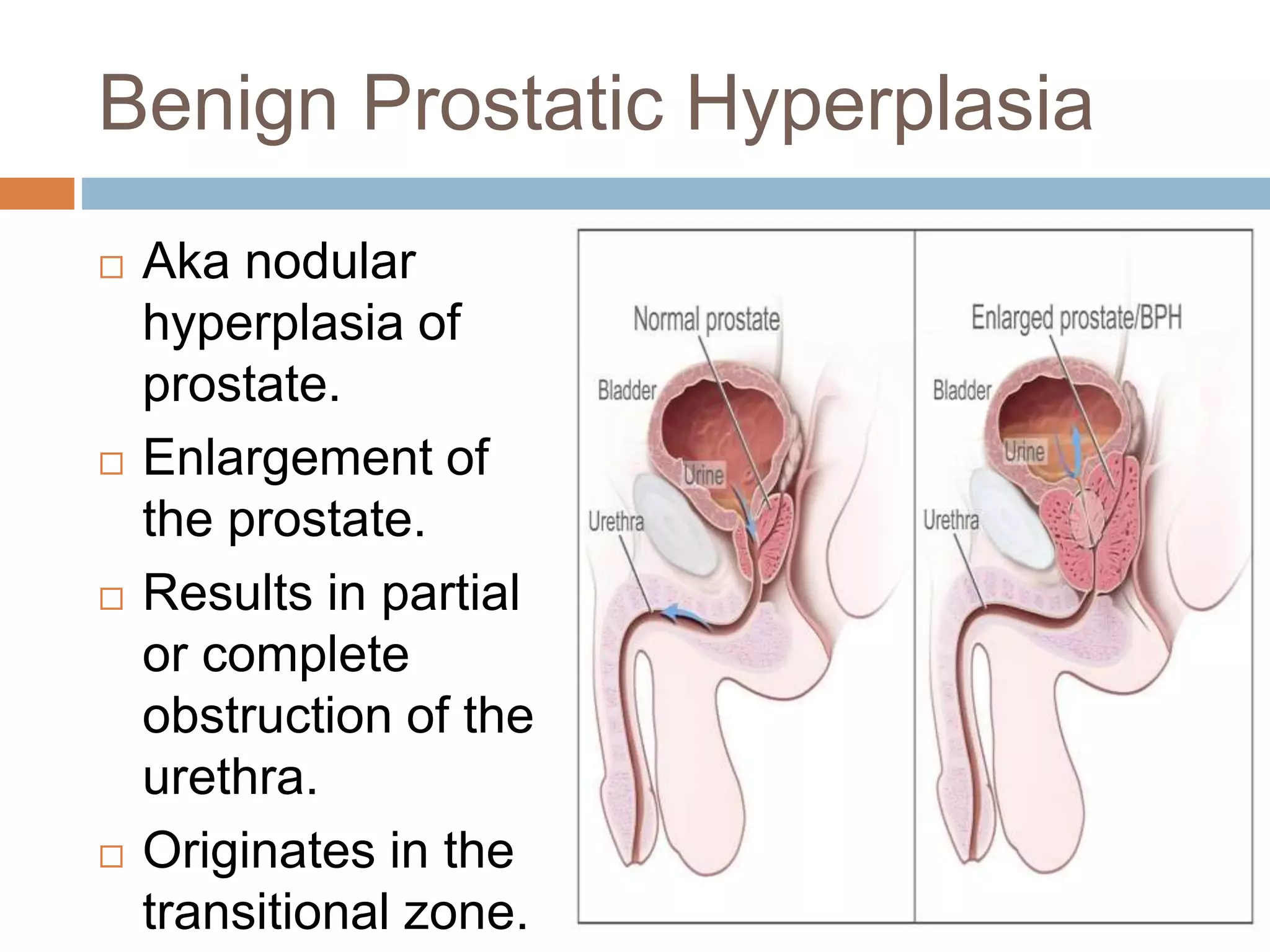
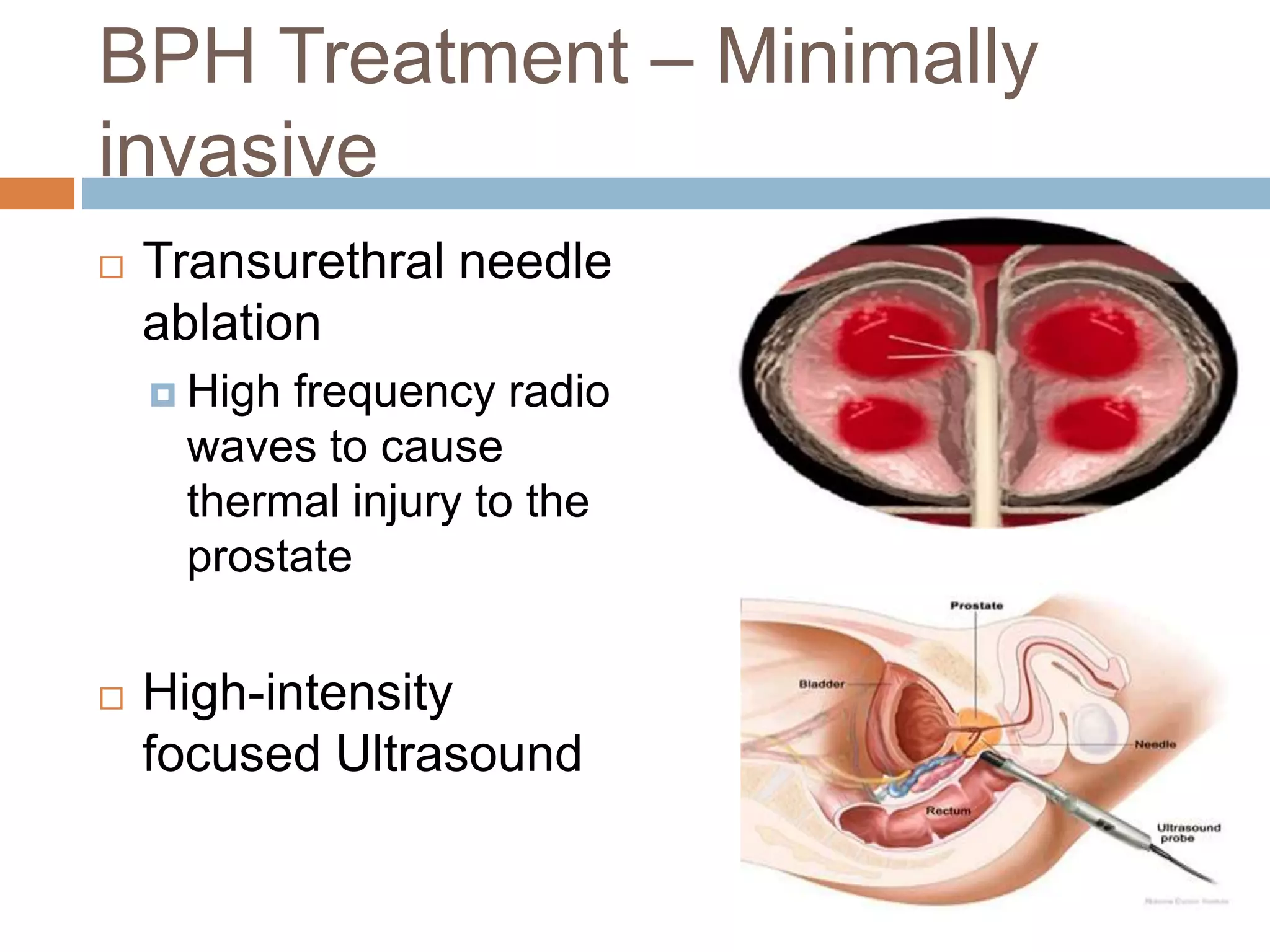
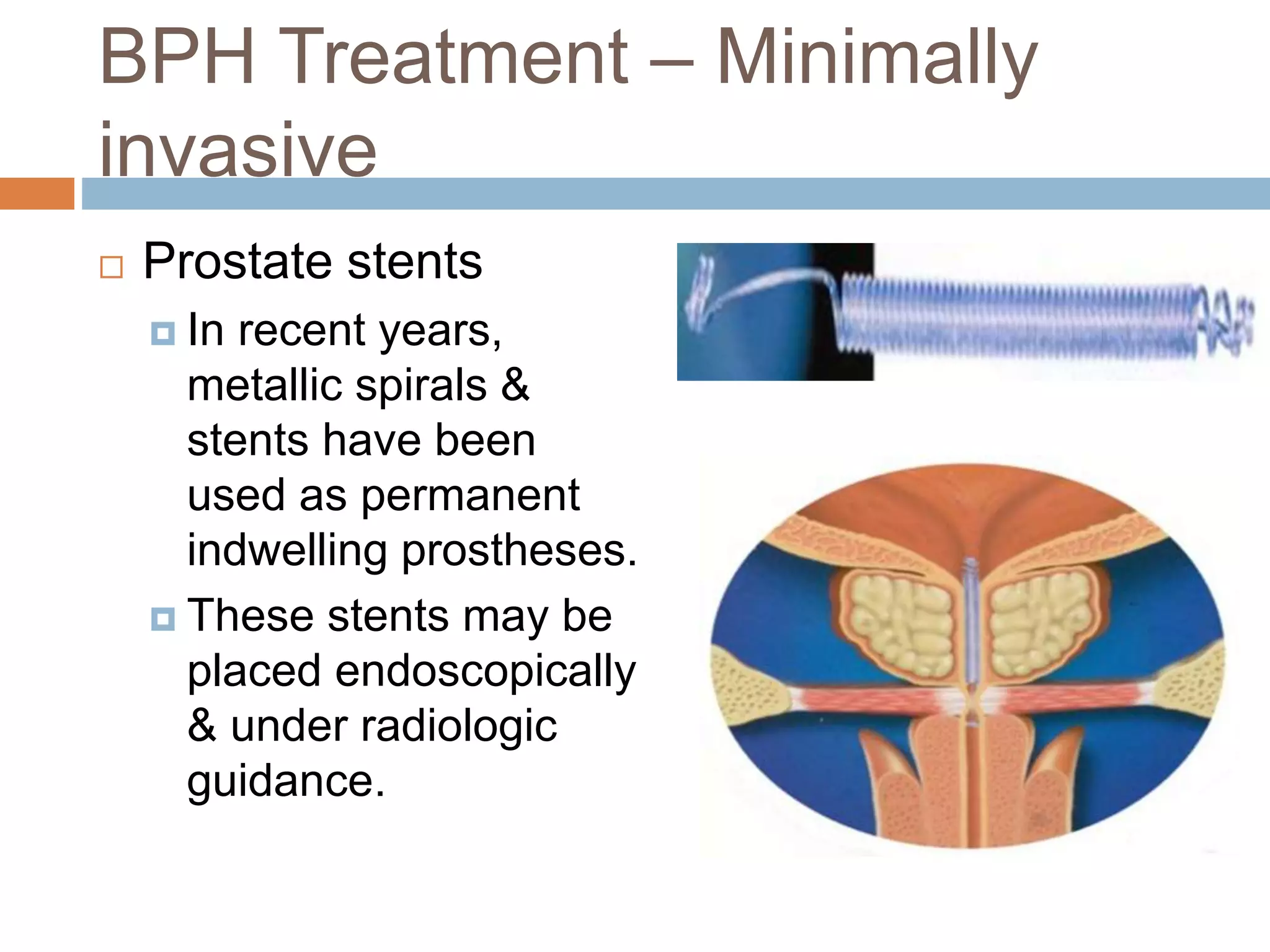
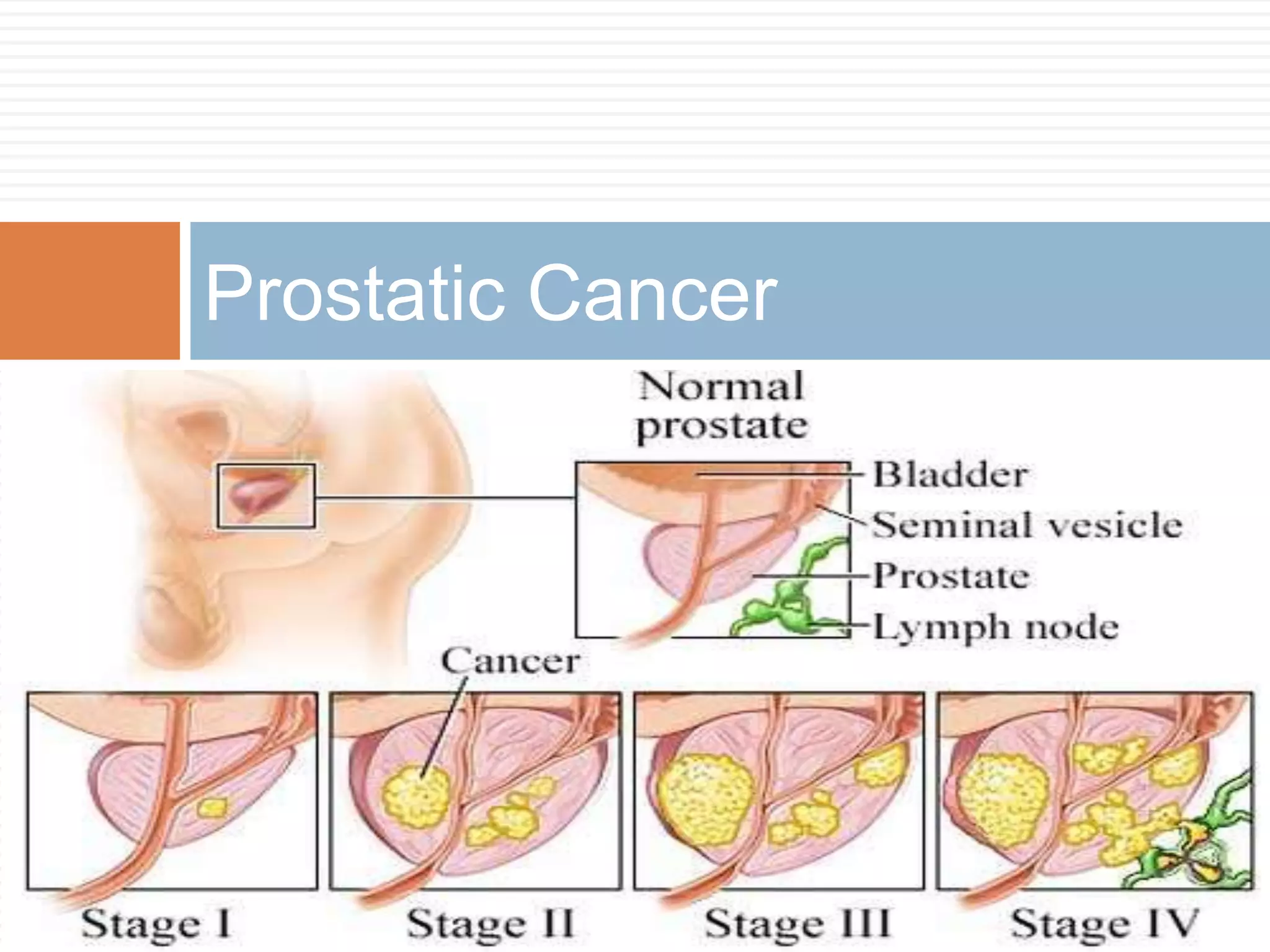
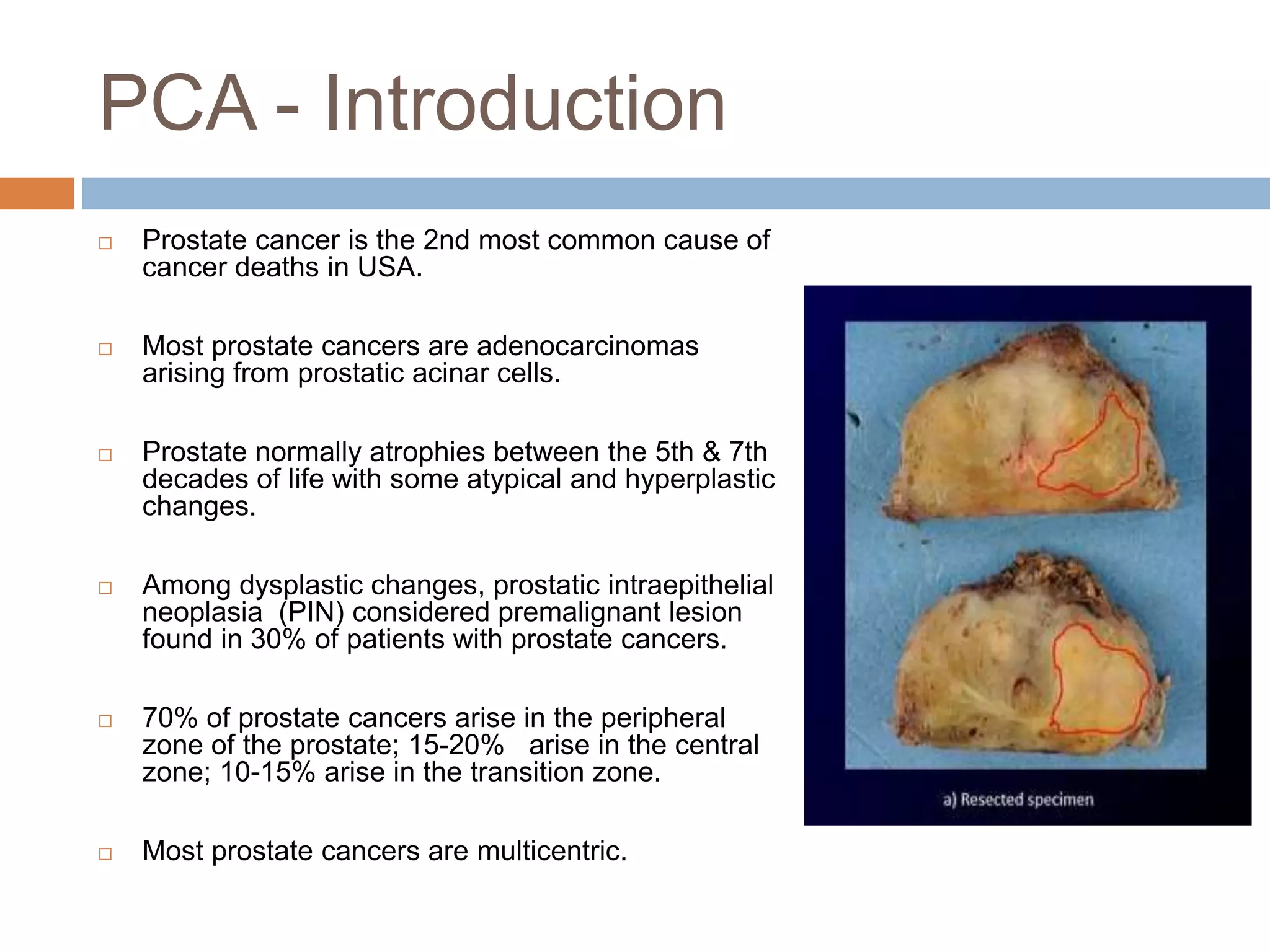
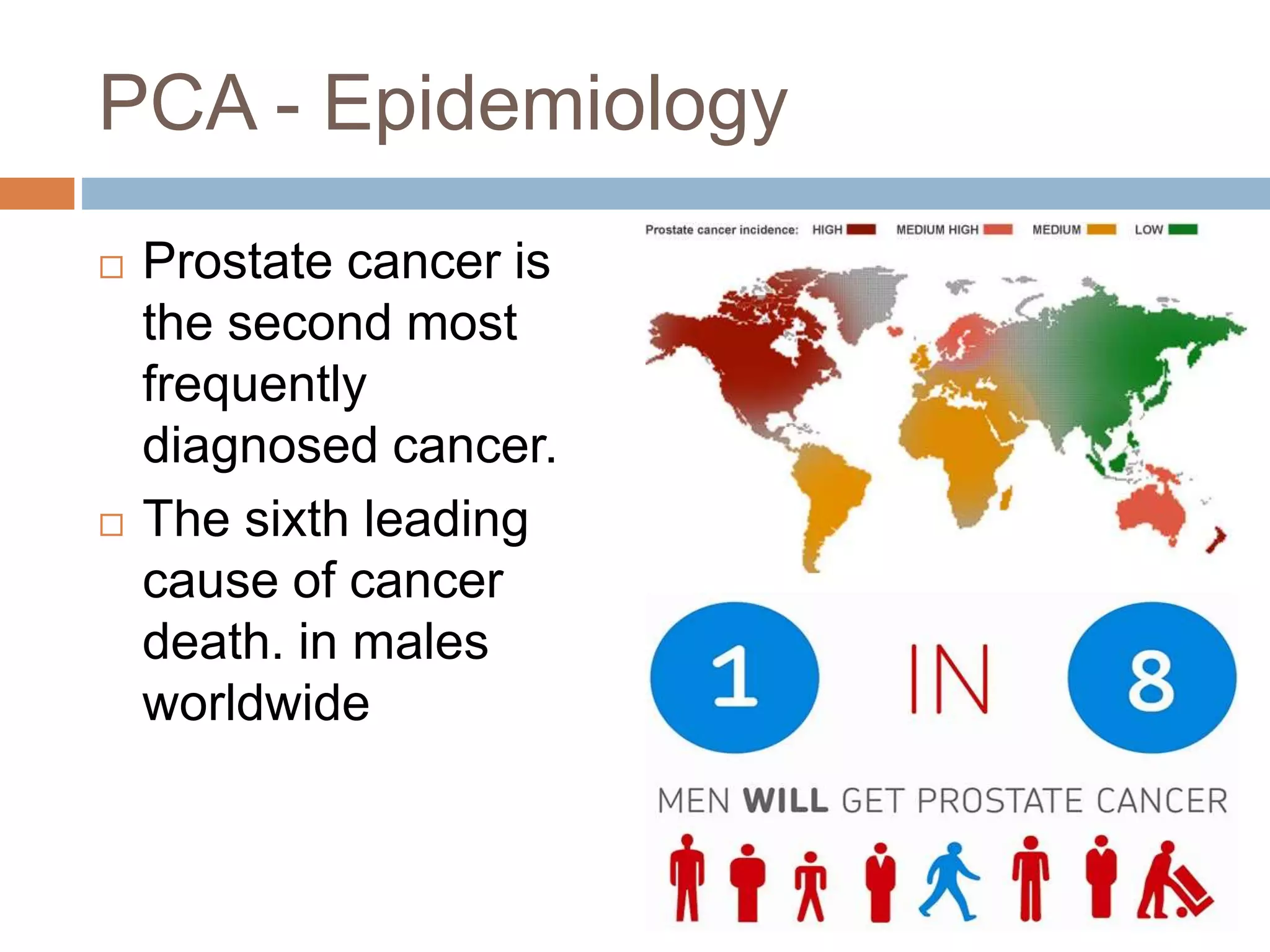
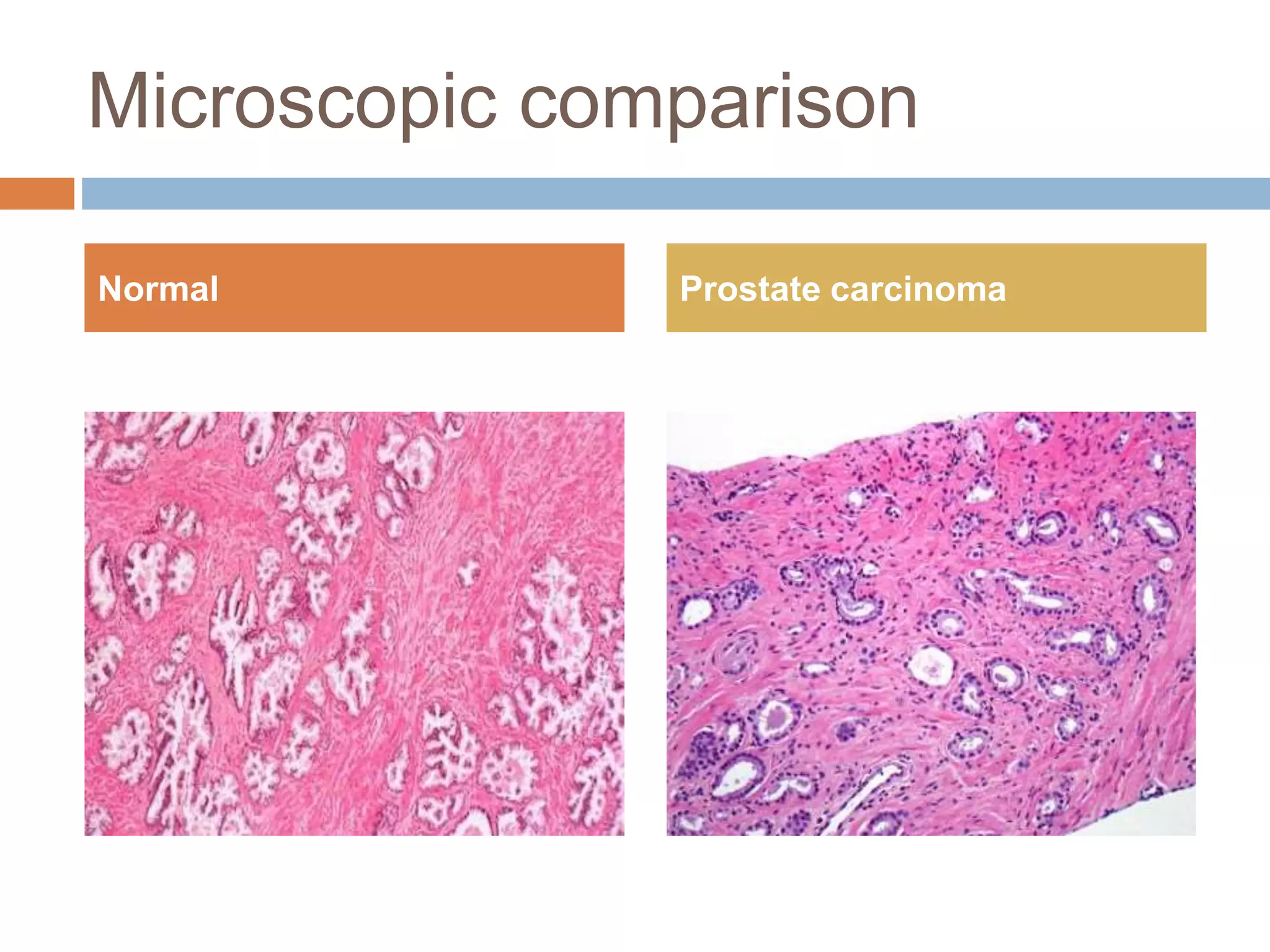
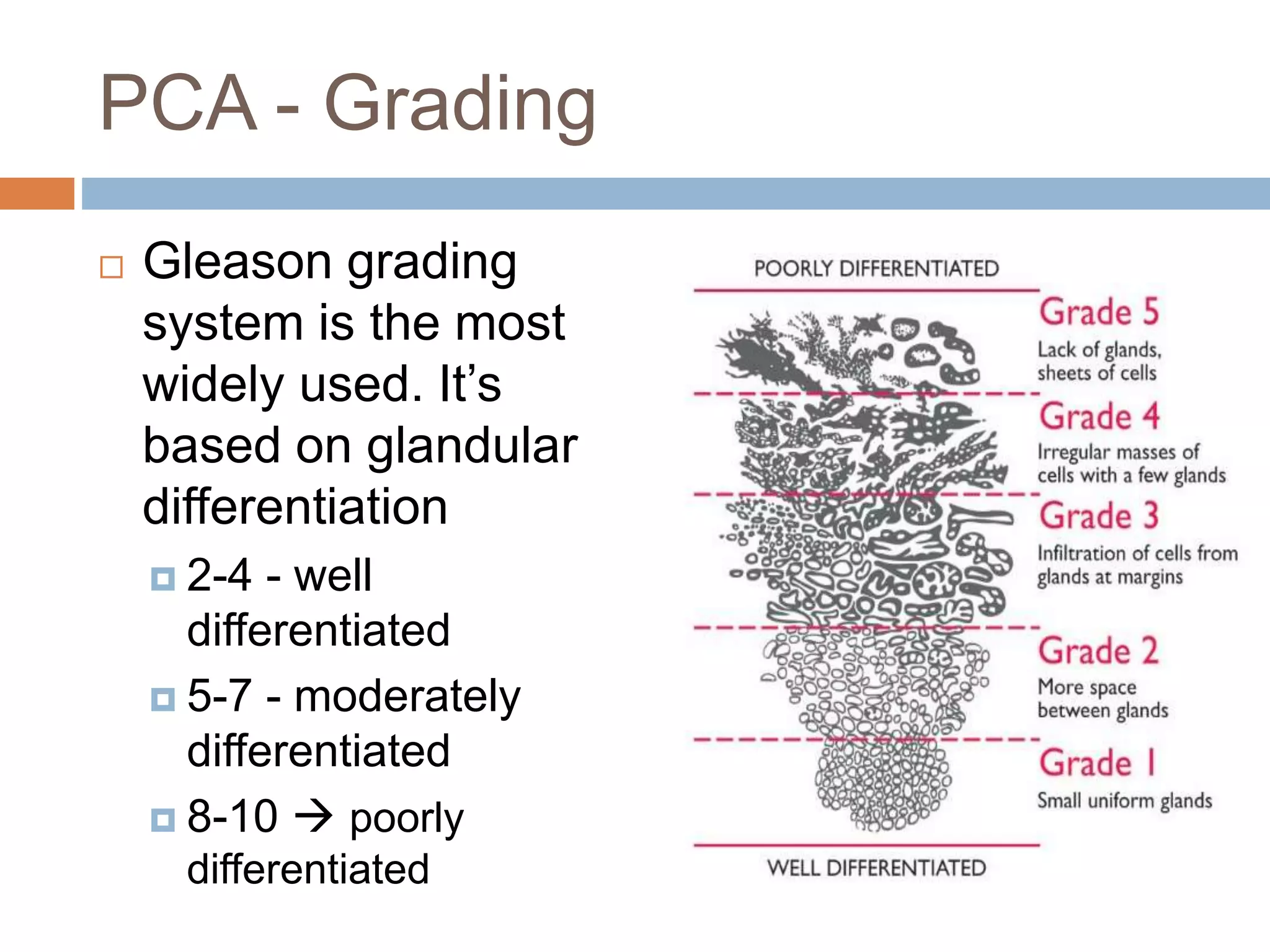
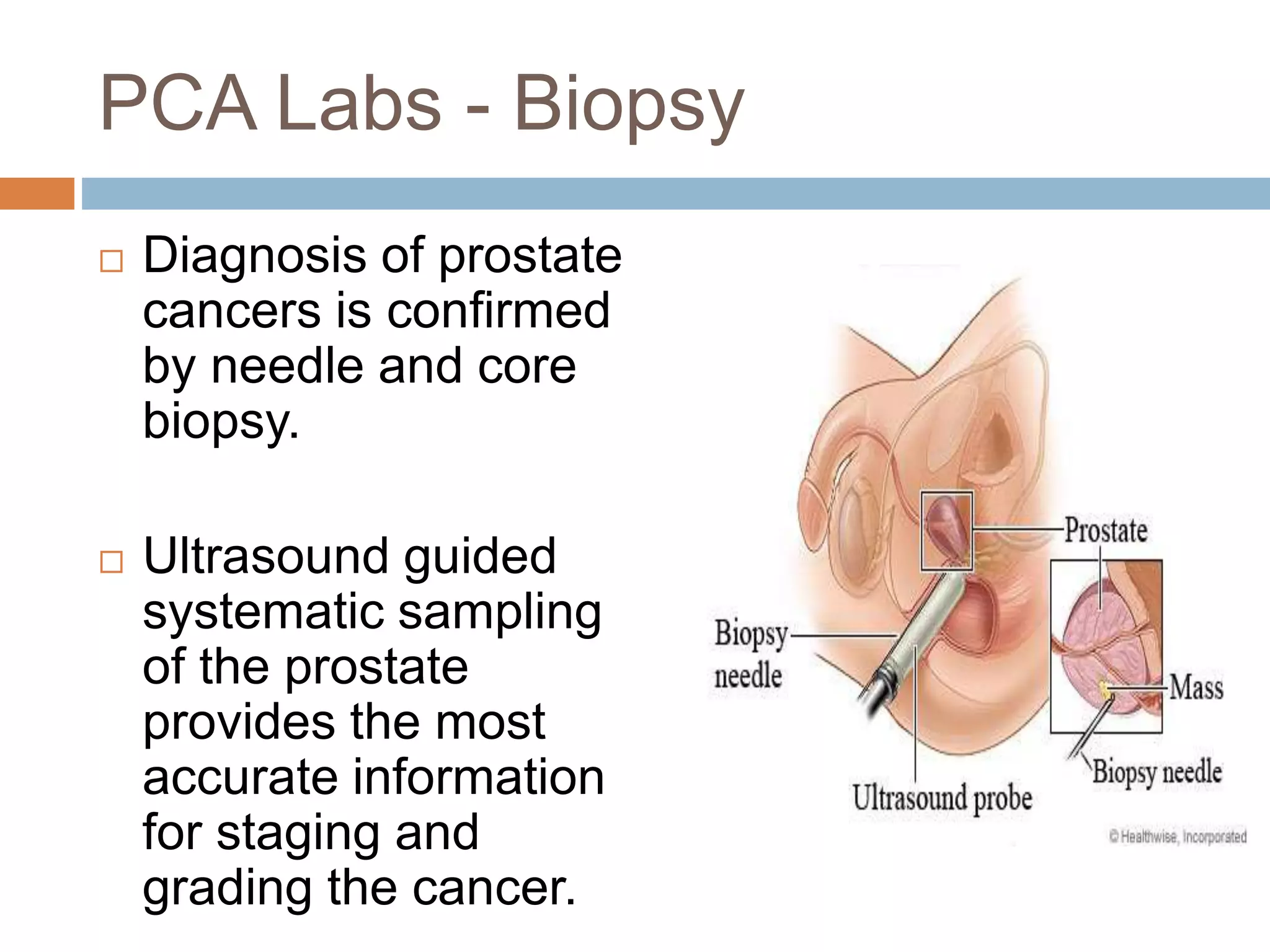
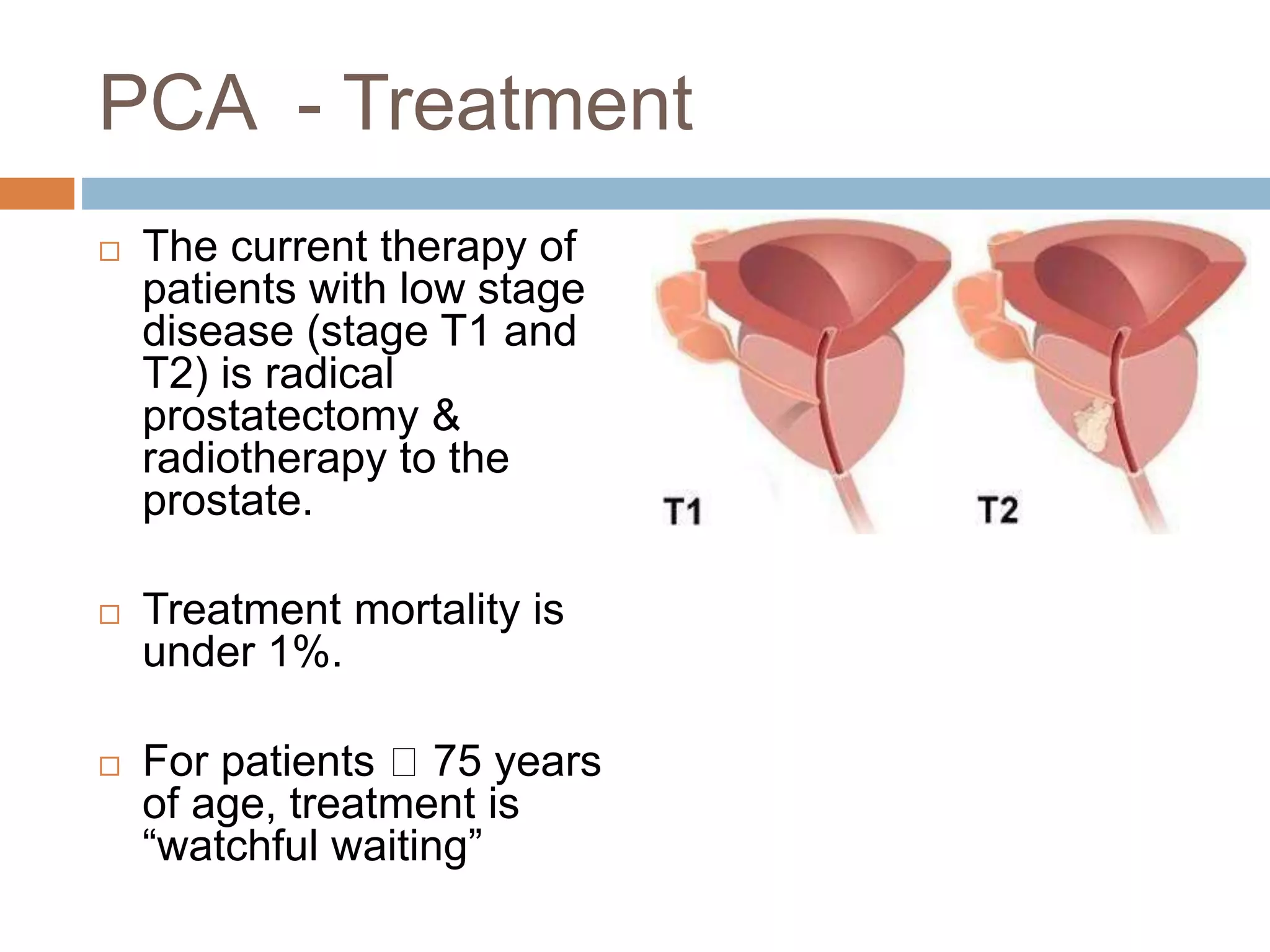
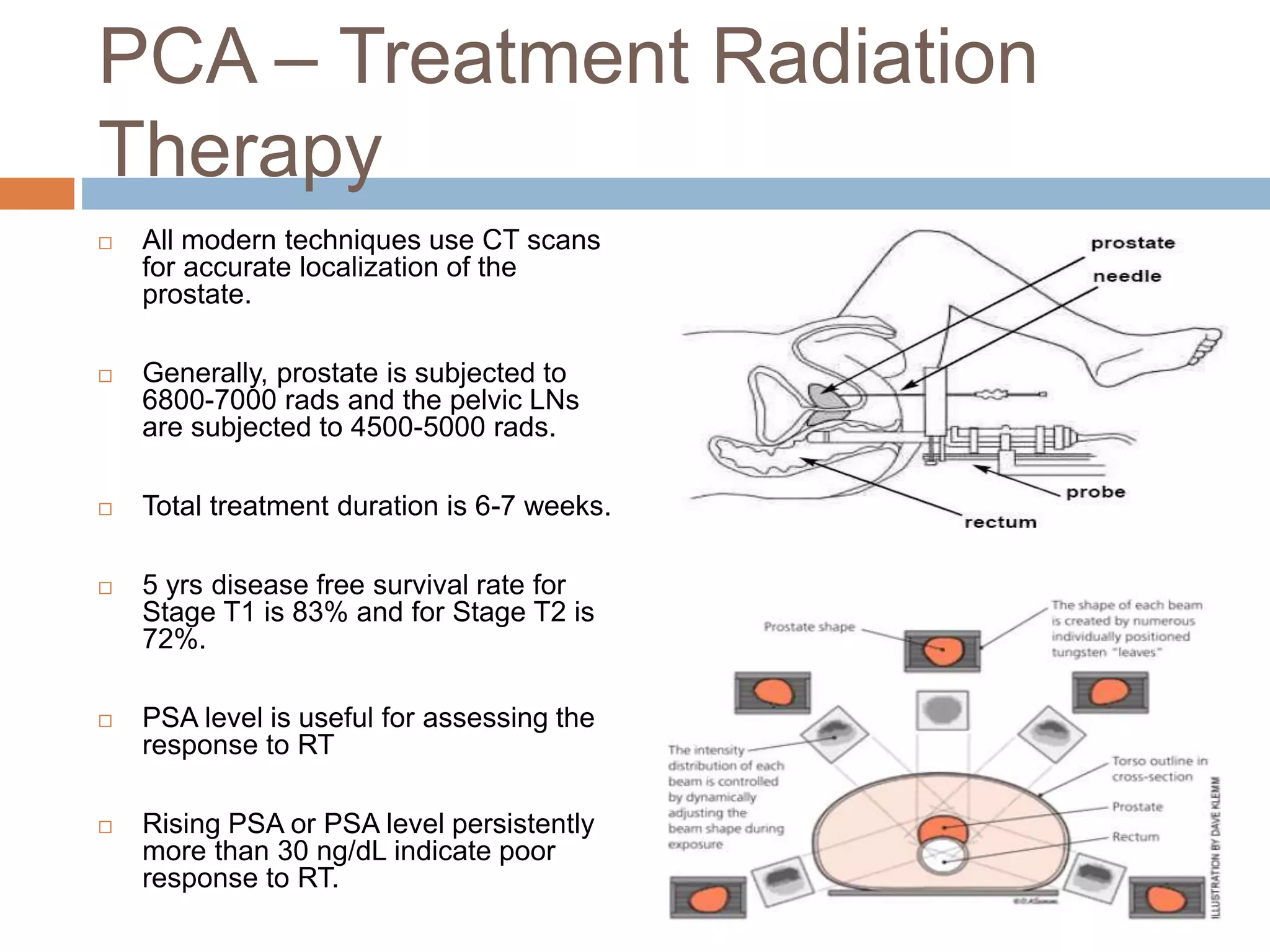
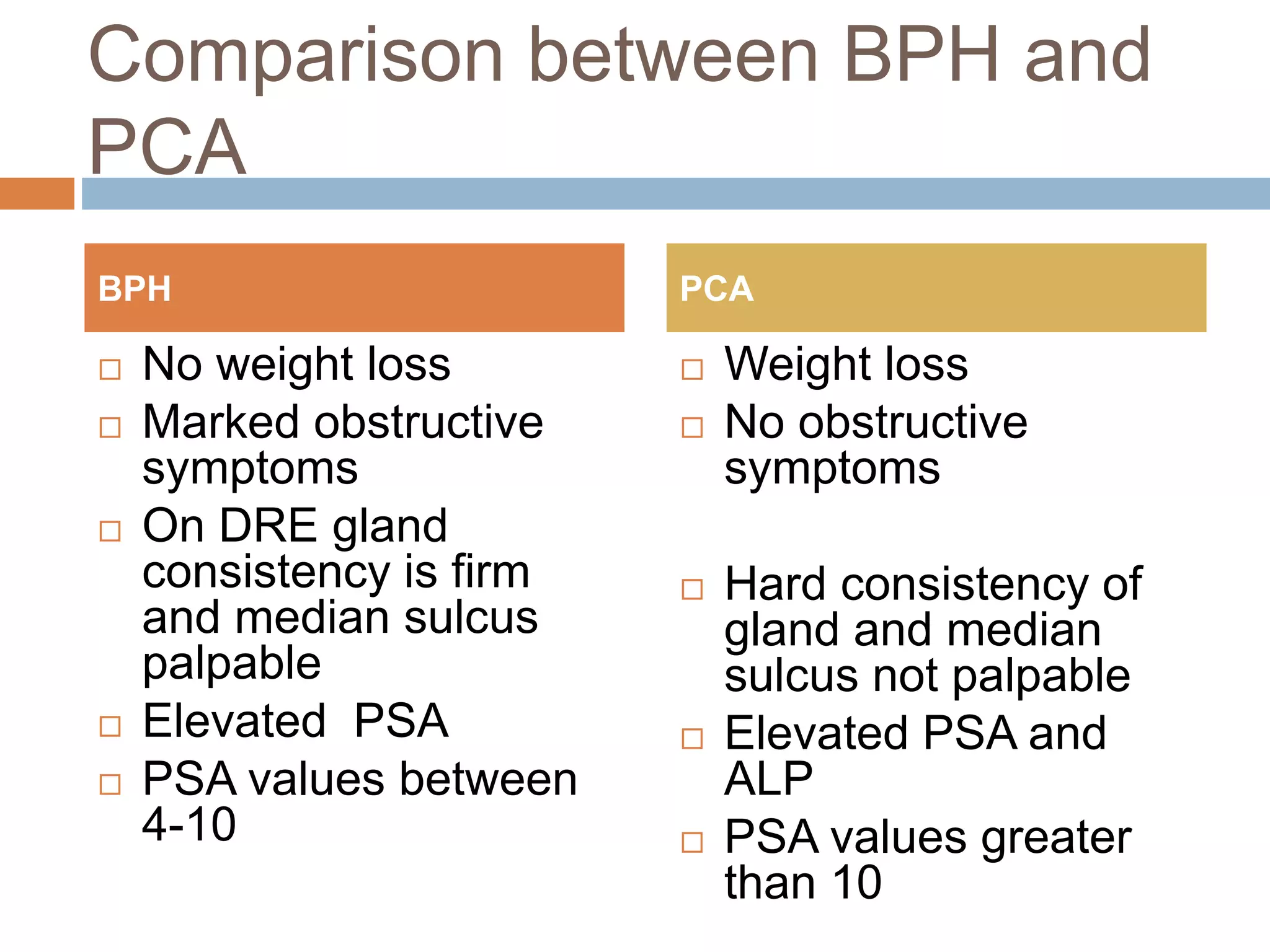
The document provides a comprehensive overview of the prostate, detailing its anatomy, functions, benign prostatic hyperplasia (BPH), and prostate cancer (PCA). It discusses symptoms, diagnosis, and treatments for both conditions, emphasizing the differences between BPH and PCA in terms of symptoms, PSA levels, and examination findings. The document also highlights the importance of understanding the neurovascular supply and pathophysiology of these conditions in the context of male reproductive health.