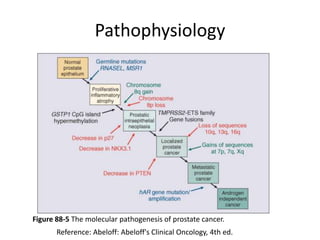
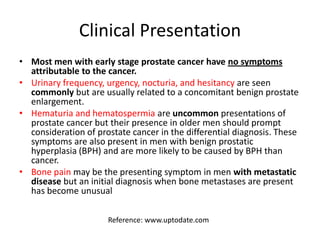
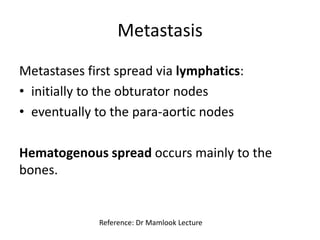
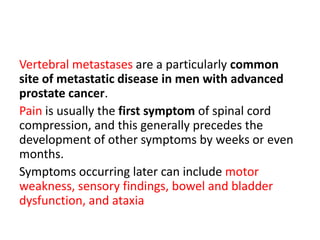
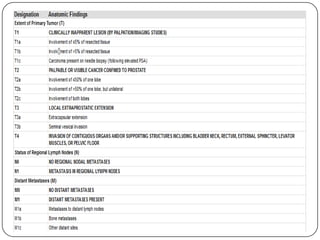
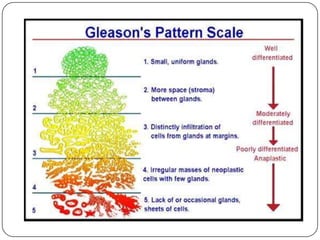
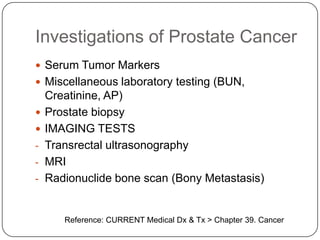
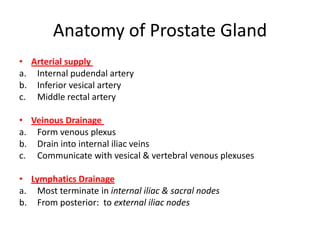
This document provides an overview of prostate cancer, including the anatomy and histology of the prostate gland, risk factors for prostate cancer such as age and family history, common symptoms and sites of metastasis, methods of grading and staging prostate cancer, investigations used in diagnosis, and management options. The pathophysiology involves genetic mutations and hormonal influences on prostate cell growth. Treatment may include radical prostatectomy, radiation therapy, surveillance, or a combination of therapies.
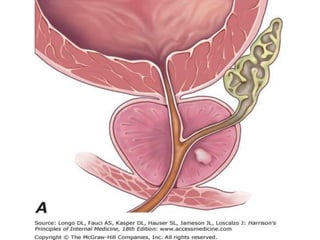
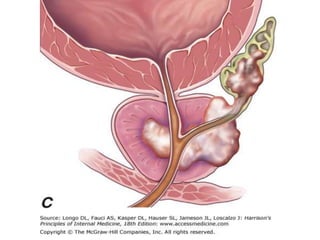
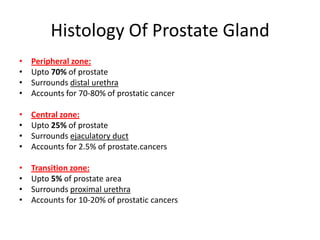
![Figure - Zones of the prostate. The peripheral zone, accounting for of the prostate gland, is the site of origin of ≤ of prostate cancers; the central zone,
approximately of the prostate gland, gives rise to only to of prostate cancers; and the transition zone, ∼ to of the prostate gland, gives rise to of
prostate cancers and is the site of origin of benign prostatic hyperplasia (BPH
(From Green DR, Shabsign R, Scardino PT: Urological ultrasonography. In: Walsh PC, Rettic AB, Stamey CA, Vaughan ED Jr [eds]: Campbells's Textbook of Urology,
th ed. Philadelphia, WB Saunders,](https://image.slidesharecdn.com/6-prostatecancer-130419171044-phpapp02/85/Prostate-Cancer-5-320.jpg)

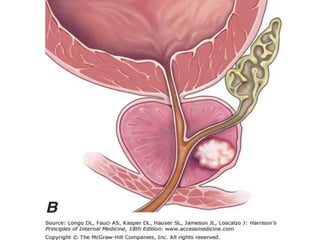
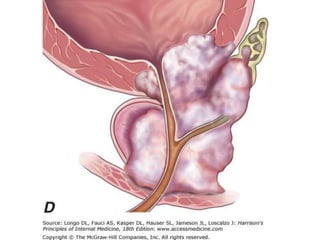
![Figure 91–2 Testosterone (T) diffuses into the prostate epithelial and stromal cell. T can interact directly with the androgen (steroid) receptors bound to the promoter
region of androgen-regulated genes. In the stromal cell a majority of T is converted into dihydrotestosterone (DHT)—a much more potent androgen—which can act in
an autocrine fashion in the stromal cell or in a paracrine fashion by diffusing into epithelial cells in close proximity. DHT produced peripherally, primarily in the skin
and liver, can diffuse into the prostate from the circulation and act in a true endocrine fashion. In some cases the basal cell in the prostate may serve as a DHT
production site, similar to the stromal cell. Autocrine and paracrine growth factors may also be involved in androgen-dependent processes within the prostate.
(From Roehrborn CG. Pathology of benign prostatic hyperplasia. Int J Impot Res 2008;20[Suppl. 3]:S11–8.)](https://image.slidesharecdn.com/6-prostatecancer-130419171044-phpapp02/85/Prostate-Cancer-12-320.jpg)