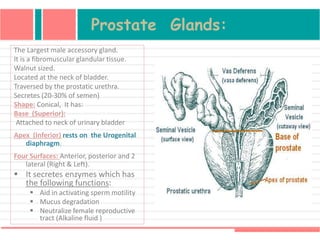
This document describes the male pelvic viscera and reproductive system. It discusses the primary sex organ (testis), reproductive tract (epididymis, vas deferens, spermatic cord), and accessory sex glands (seminal vesicles, prostate, bulbourethral glands). It also describes the external genitalia including the penis, scrotum, testes and their coverings and vasculature. Accessory glands like the seminal vesicles and prostate are also summarized, along with the structures and blood supply of the penis.