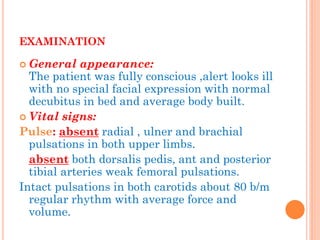
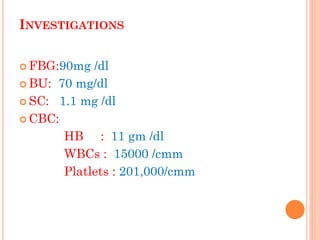
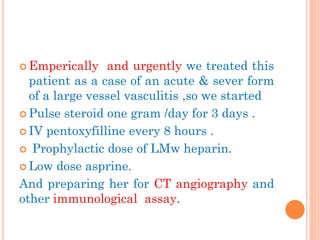
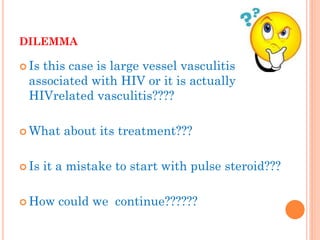
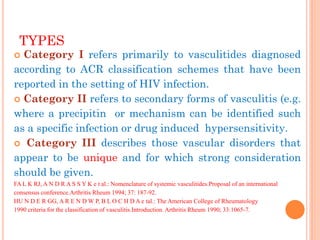
A 47-year-old female presented with acute severe pain in her limbs. Examination found absent pulses. Imaging showed diffuse narrowing of arteries without atherosclerosis. She was found to be HIV positive and on antiretroviral therapy. Her condition improved with steroids. HIV can cause various types of vasculitis. This case represents a large vessel vasculitis seen in HIV, termed Category III, which is a distinct clinical entity associated with HIV. Treatment involves steroids and antiretrovirals.