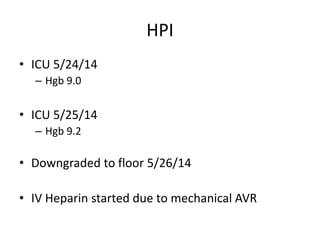
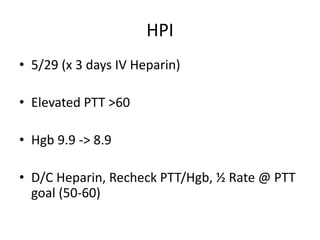
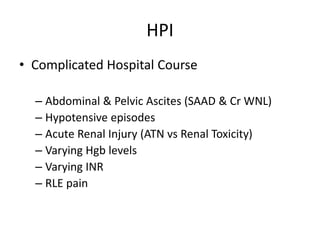
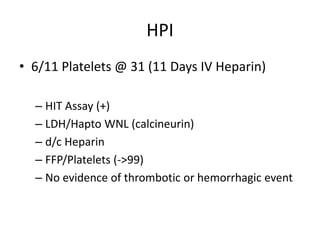
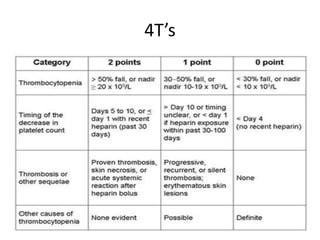
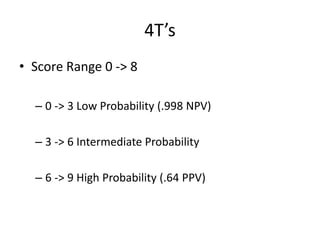
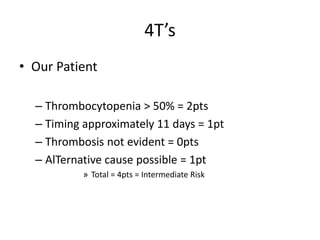
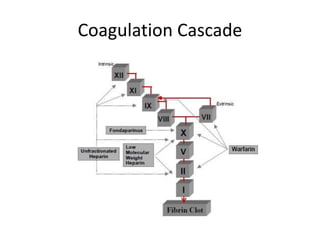
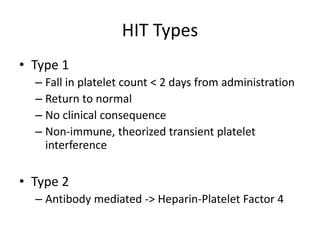
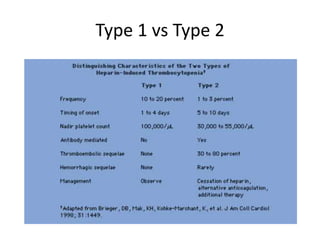
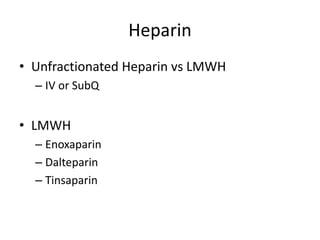
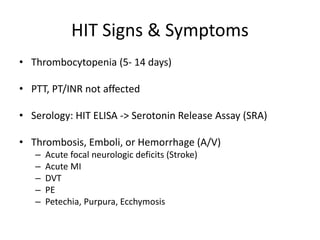
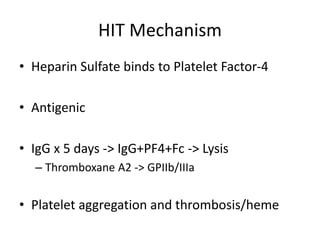
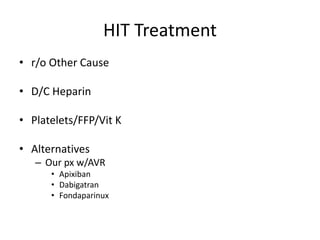
This document discusses a case of potential heparin-induced thrombocytopenia (HIT) in a 43-year-old male patient who underwent a kidney and pancreas transplant. After being started on IV heparin due to his mechanical aortic valve, his platelet count dropped to 31 after 11 days of heparin treatment. A HIT assay was positive. Heparin was discontinued and alternatives like apixiban and fondaparinux were considered due to his aortic valve replacement.