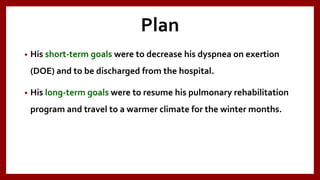
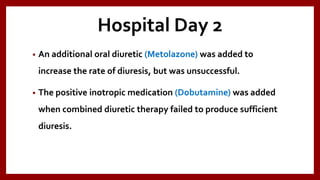
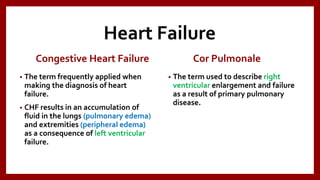
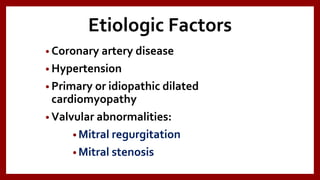
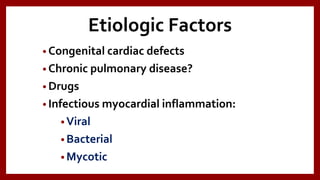
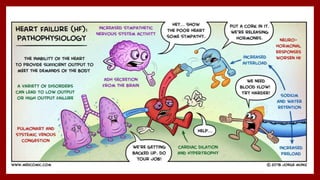
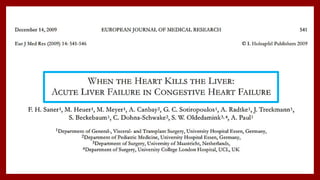
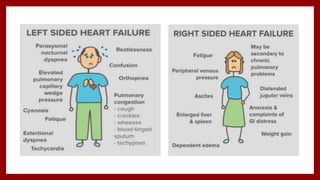
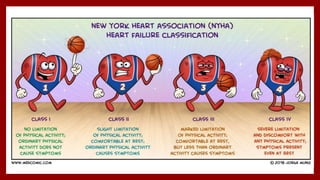
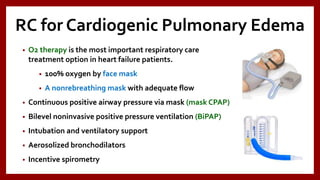
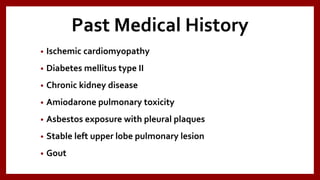
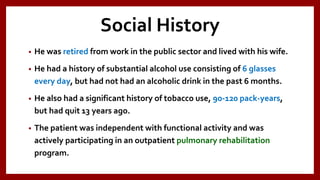
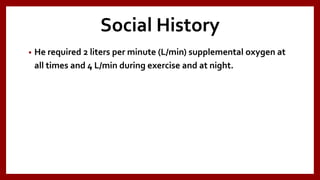
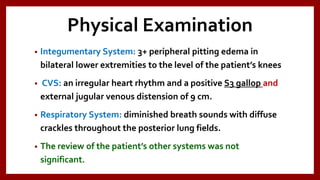
The document presents a detailed overview of heart failure, including its definitions, causes, risk factors, pathophysiology, signs and symptoms, investigations, and treatment options. It includes a case study of a 67-year-old man with ischemic cardiomyopathy, who experienced symptoms of acute decompensated heart failure and underwent various treatments, ultimately leading to a decrease in weight and improvement in symptoms. The document emphasizes the importance of respiratory care management in patients with cardiogenic pulmonary edema, highlighting specific therapeutic interventions.




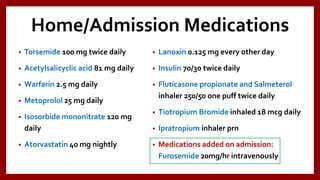
![Chest X-Ray
• Cardiomegaly
• Cephalization of blood flow
• Kerley’s A lines [1- to 2-cm lines of
interstitial edema out from the hilum]
• Kerley’s B lines [short, thin, flattened
streaks of interstitial edema outlining
the subsegmental lymphatics that
extend from the pleural surface]](https://image.slidesharecdn.com/heartfailure-180328114636/85/Heart-Failure-Case-Presentation-18-320.jpg)



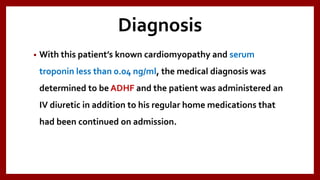
![Baseline PFT prior to
hospitalization
• (Pre-bronchodilator):
• FEV1= 1.13L (34%)
• FVC= 1.50L (35%)
• FEV1/FVC= 75% (96%)
• TLC= 2.21L (34%)
• (DLCO)Test [hemoglobin] = 8.72 (33%) mL/min/mm Hg](https://image.slidesharecdn.com/heartfailure-180328114636/85/Heart-Failure-Case-Presentation-39-320.jpg)