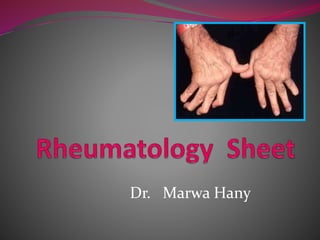
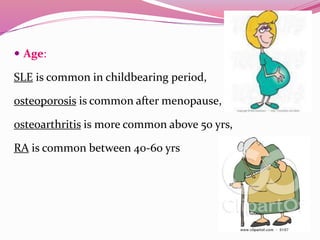
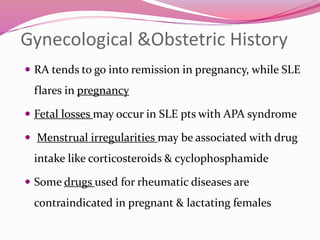
The document provides an in-depth overview of rheumatic diseases, including classifications, types, and important clinical history-taking aspects. It details various conditions such as rheumatoid arthritis, osteoarthritis, and lupus, along with the significance of personal history, symptoms, and examinations in diagnosing these diseases. The comprehensive approach emphasizes the necessity for early intervention and tailored care for patients with rheumatological conditions.