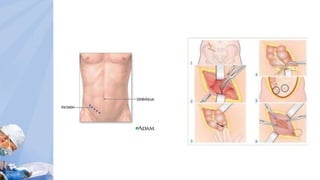
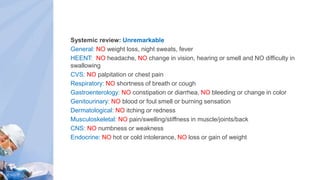
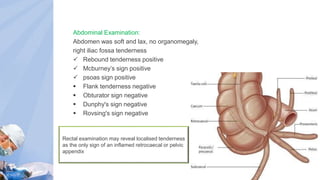
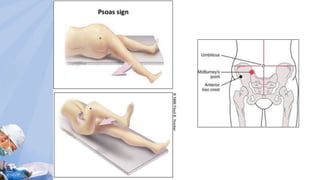
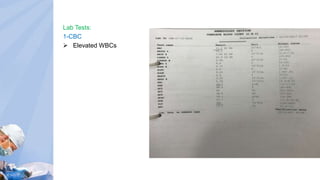
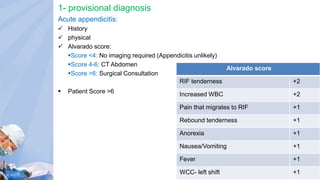
Turki Ali Ahmed, a 37-year old Saudi male, presented to the emergency room with sharp right lower quadrant pain for two days. On examination, he had tenderness in the right lower quadrant with rebound and other signs positive for acute appendicitis. Laboratory tests showed elevated white blood cell count. The differential diagnosis included appendicitis, testicular torsion, urinary tract infection, kidney stones, and inflammatory bowel disease. Given the clinical findings, appendicitis was considered provisional. The patient was admitted for IV fluids, NPO status, and pre-op management. He then underwent an open appendectomy and was started on IV antibiotics and pain medications post-surgery.






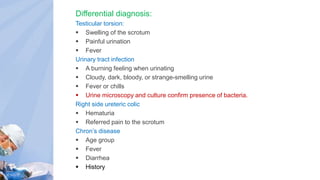
![Management:
Admit the patient
1- Stabilize
IVF (D5 1L) + (NS 120ml/h)
2-Monitor
NPO
Pre op
Anesthesia [omeprazole 40mg IV]
Antibiotics [Cefuroxime 1.5g IV on call to OR]
3-surgery
open appendectomy
4- post surgery
Antibiotics:
cefuroxime750mg BID IV,
flagyl 500mg BID IV
Paracetamol
1g Q6hrs IV](https://image.slidesharecdn.com/acuteappendicitis-171119140350/85/Acute-appendicitis-Case-Presentation-16-320.jpg)