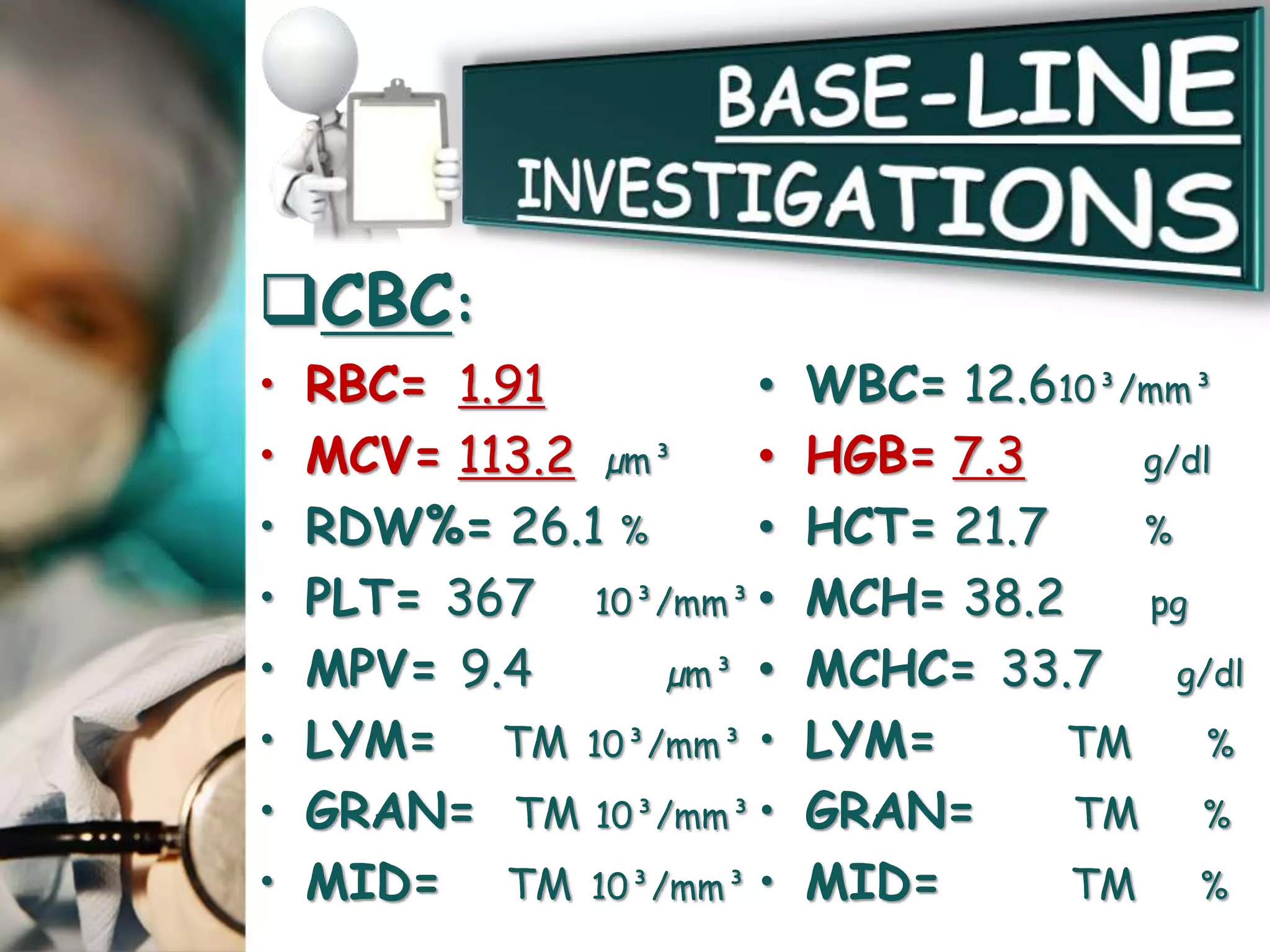
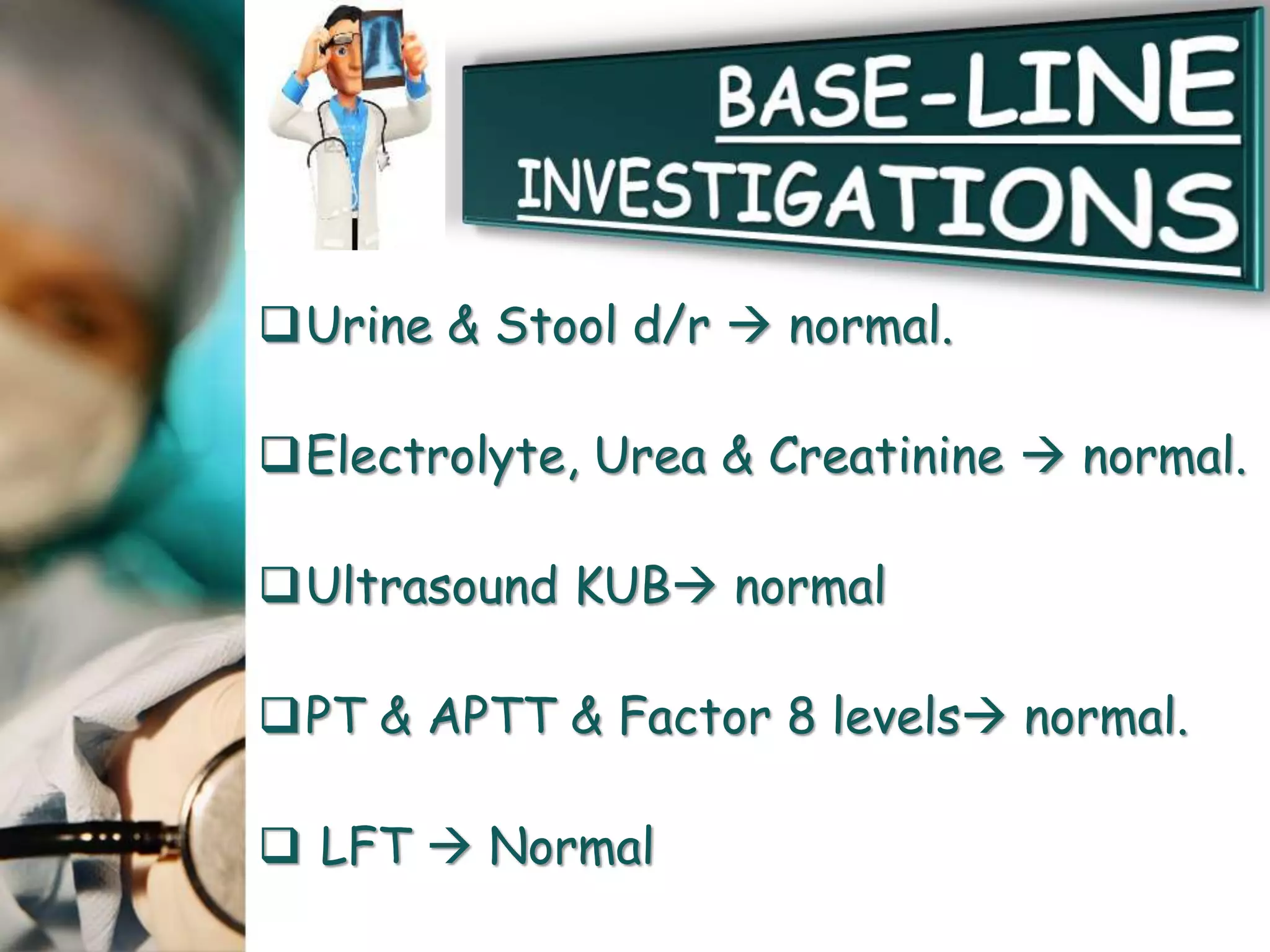
This document presents the case of a 10-year-old boy who was admitted to the hospital with recurrent illnesses over the past few months. His symptoms included fever, fatigue, dizziness, shortness of breath, weight loss, loss of appetite, loss of taste, and tingling/numbness. His medical history revealed previous episodes of bleeding and fits. Laboratory tests found macrocytic anemia with low vitamin B12 levels. Based on his strict vegetarian diet and symptoms, he was diagnosed with vitamin B12 deficiency anemia. Treatment with vitamin B12 injections led to improvement of his symptoms and normalization of red blood cell levels on follow up testing.










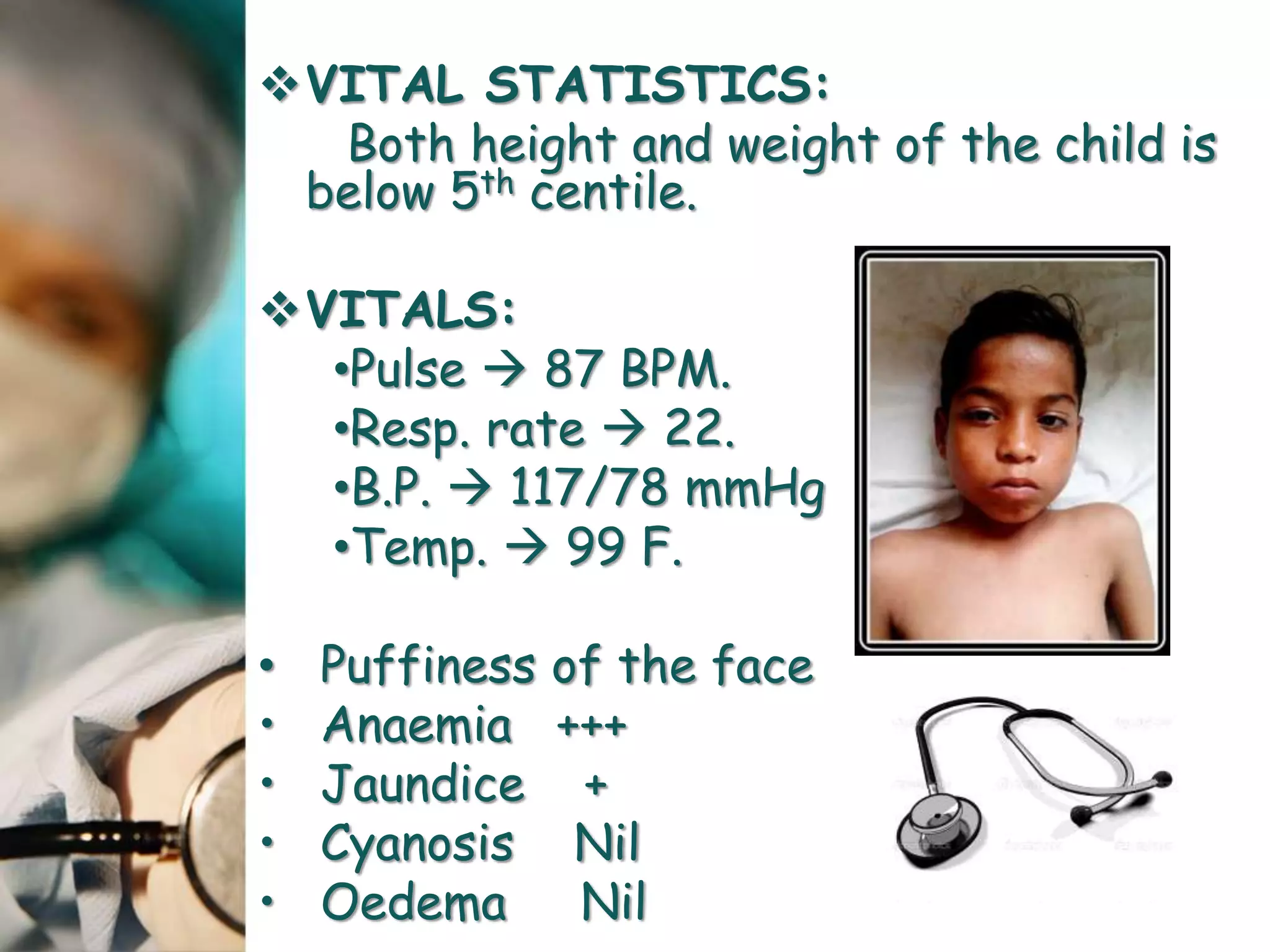







![Anaemias
• Hypochromic Microcytic
• Nutritional(Iron Deficiency Anaemia)
• Thalassaemia Major
• Thalassaemia Minor
• Chronic Blood loss
• Macrocytic
ANEMIAANEMIA
MICROCYTIC ANEMIA. [MCV <80fl]
MACROCYTIC ANEMIA. [MCV >96fl]
NORMOCYTIC ANEMIA. [MCV 80-96 fl]](https://image.slidesharecdn.com/anemia1-170328101425/75/Anemia-Case-Presentation-31-2048.jpg)