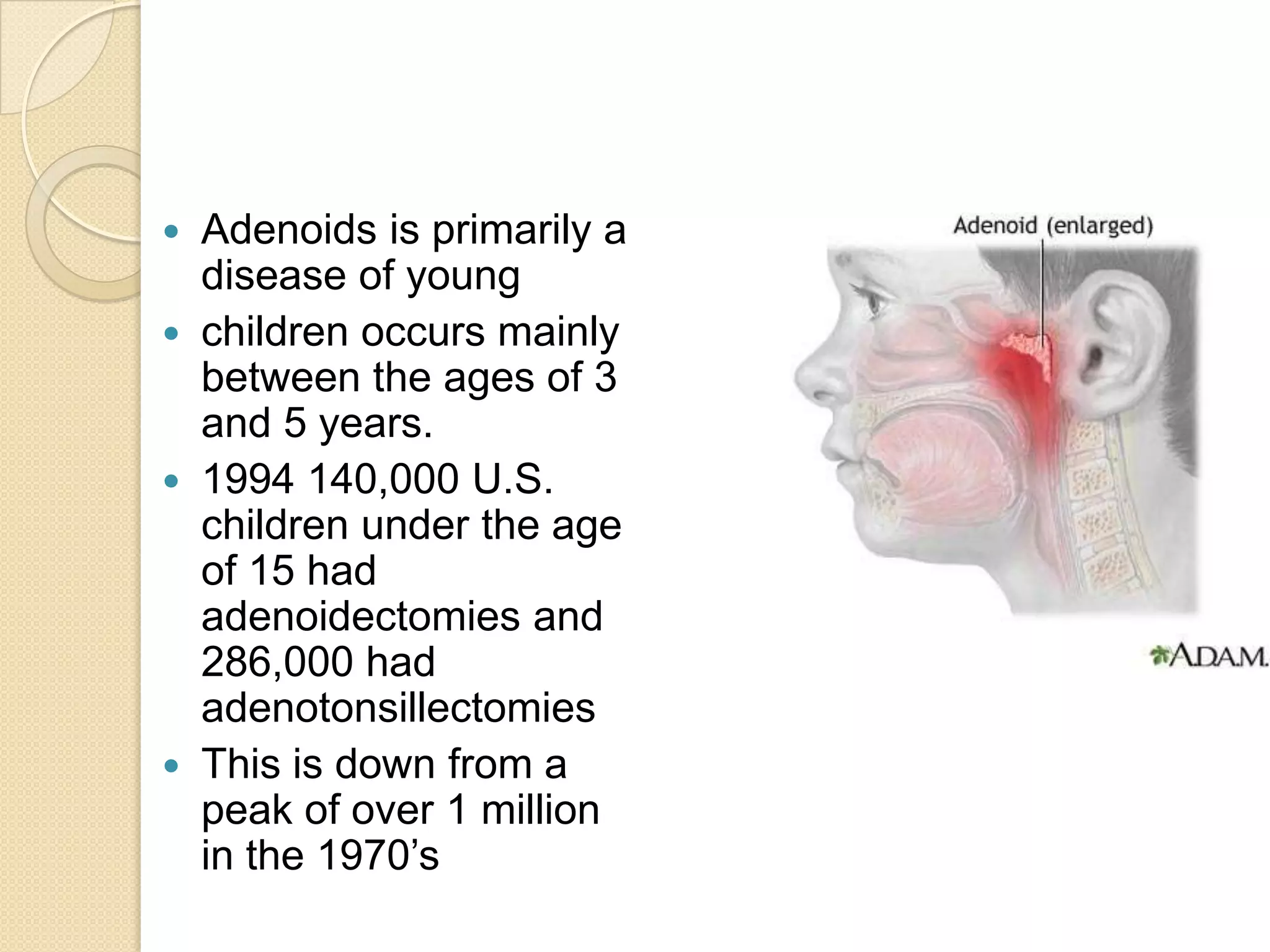
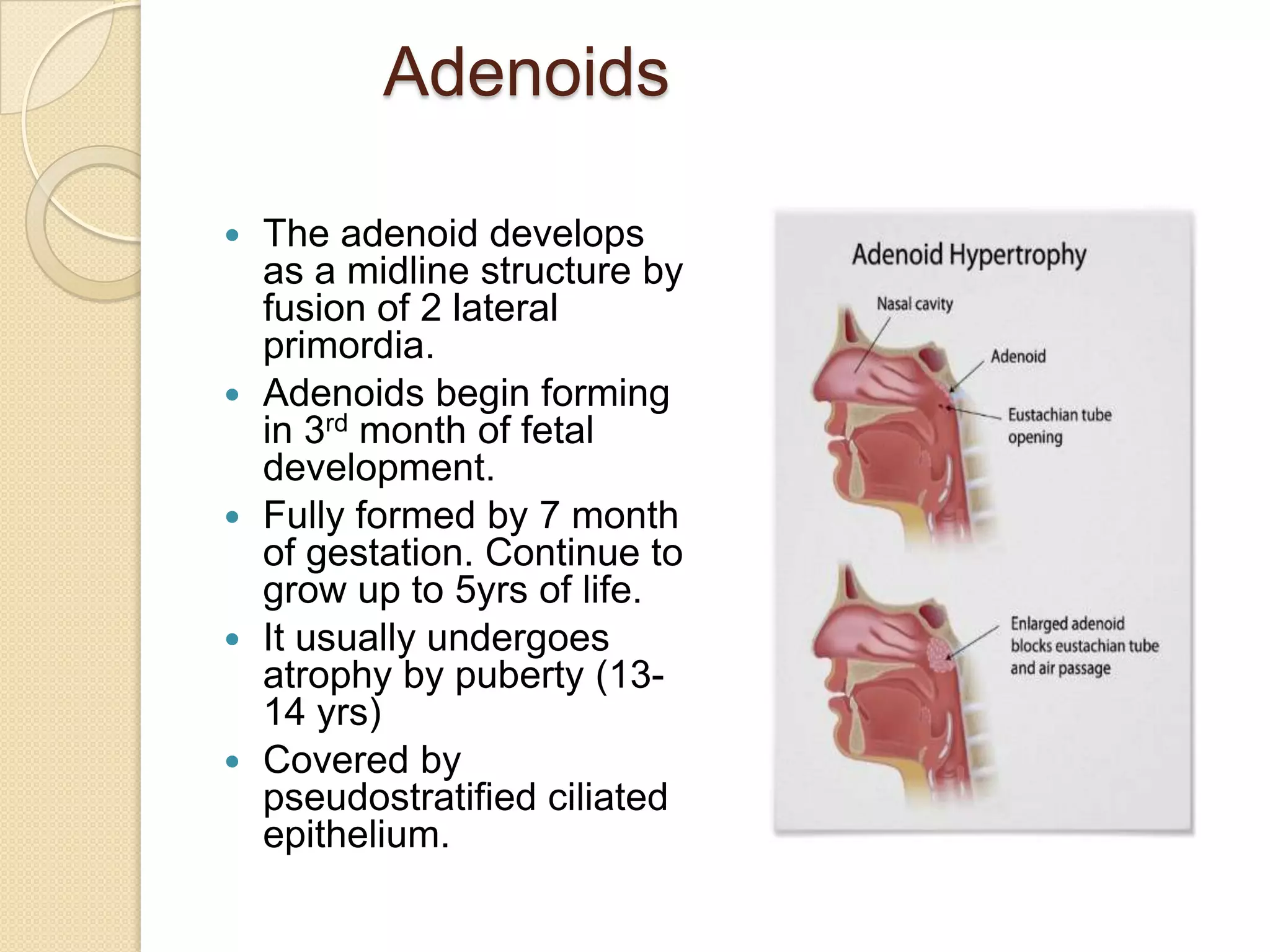
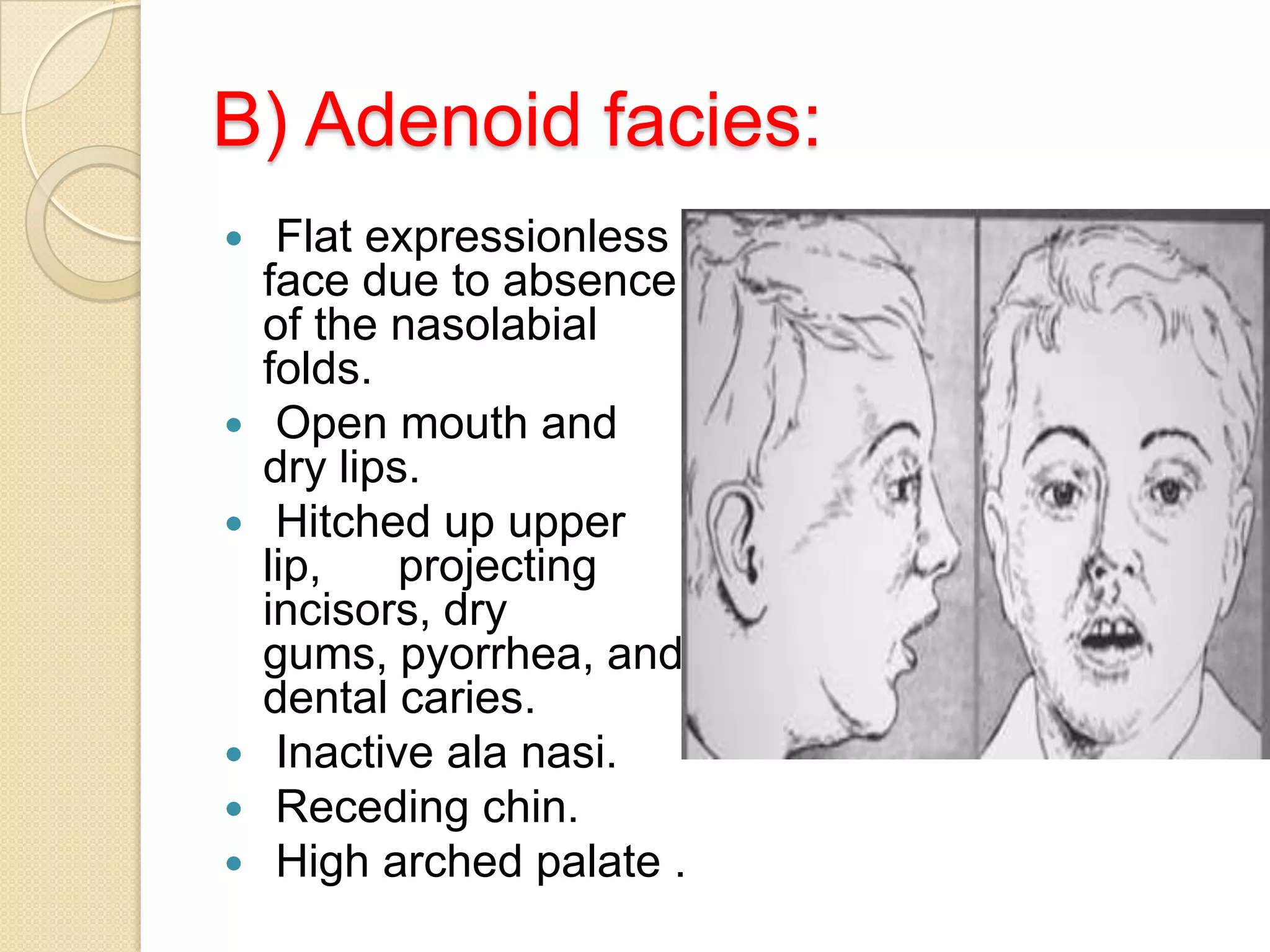
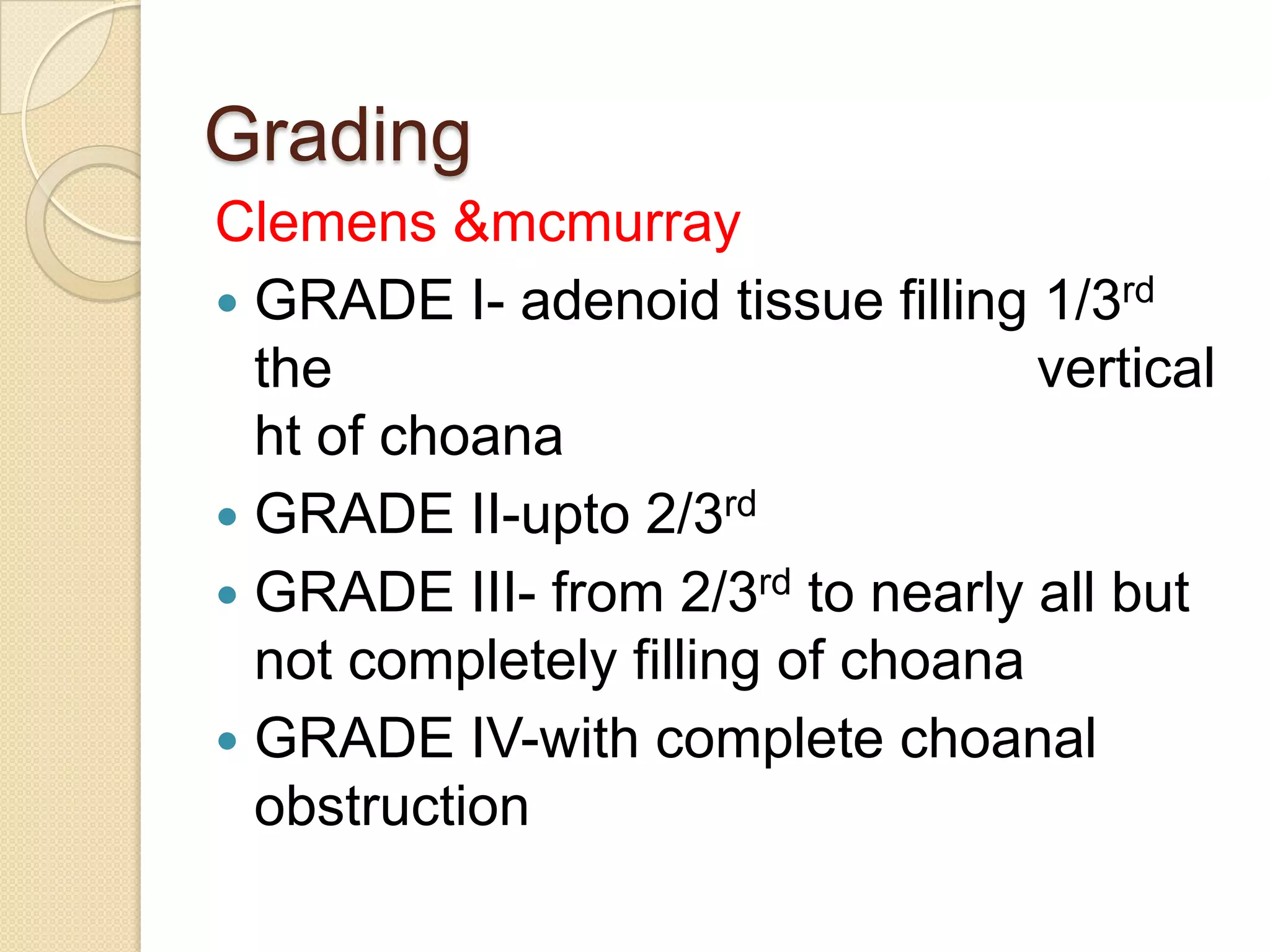
This document discusses rigid endoscopic evaluation of conventional curettage adenoidectomy. It begins with an introduction stating that adenoidectomy is a common procedure in children and conventional curettage is commonly used. It then provides details on the anatomy and physiology of the adenoids, clinical presentation of adenoid hypertrophy, diagnosis, grading systems used, different surgical techniques including conventional curettage and various types of endoscopic adenoidectomy, post-operative care, and potential complications.