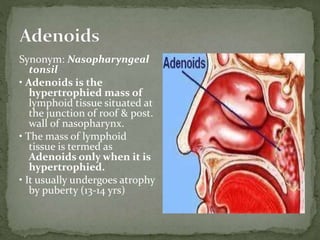
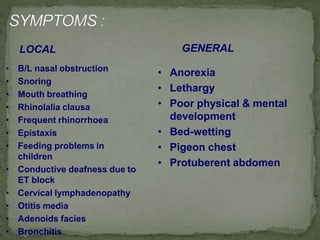
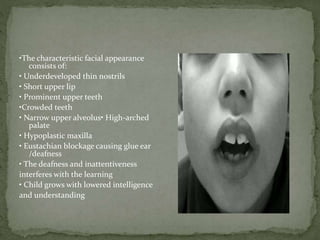
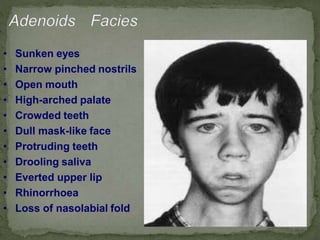
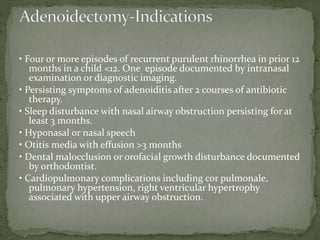
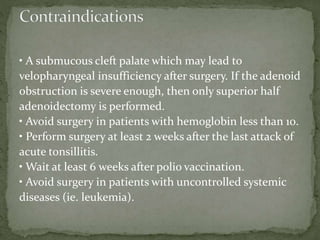
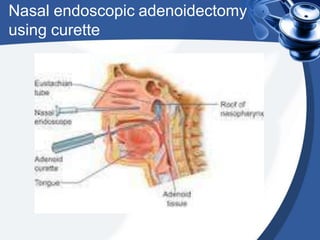
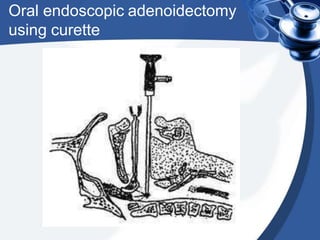
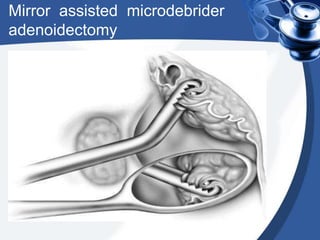
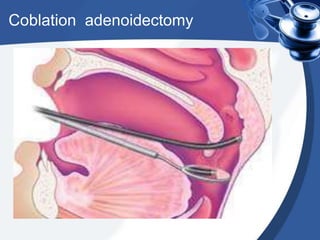
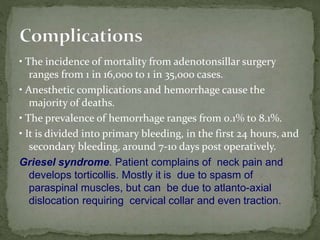
The adenoids are masses of lymphoid tissue located in the nasopharynx. They develop fully by the 7th month in utero and typically undergo involution by puberty. The adenoids play an important role in immune function but can become infected or hypertrophied, causing nasal obstruction and other symptoms. Surgical removal (adenoidectomy) using curettes or newer techniques like coblation is recommended if symptoms persist despite medical management with antibiotics or nasal steroids. Complications are rare but can include hemorrhage, airway issues, or velopharyngeal dysfunction.