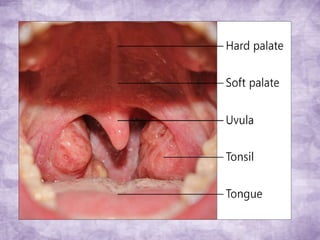
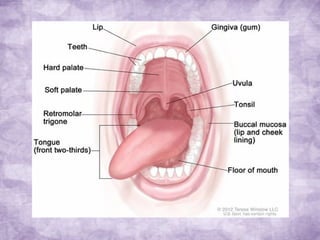
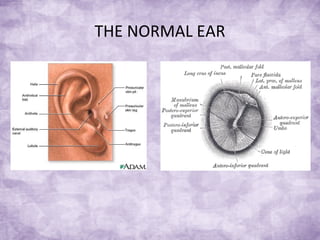
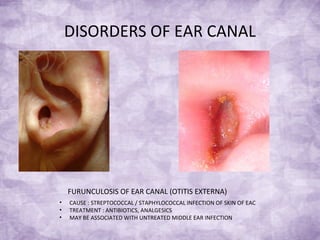
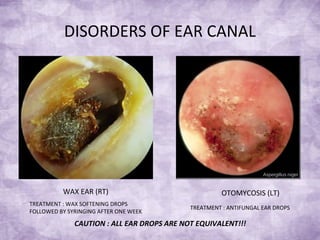
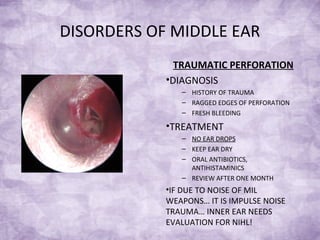
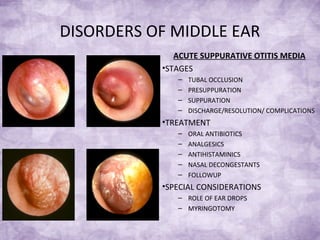
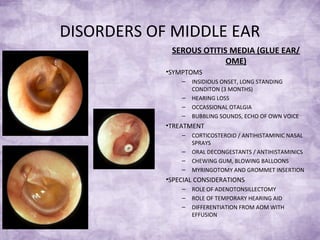
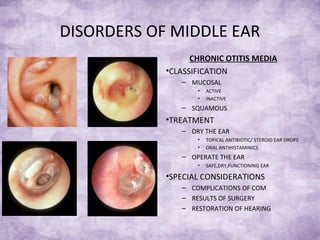
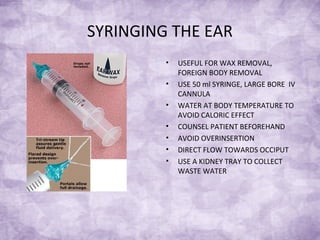
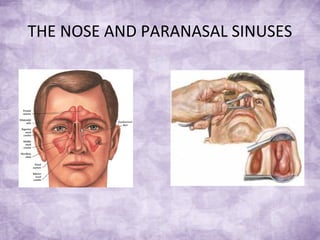
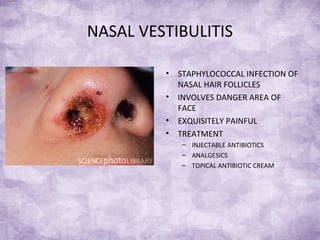
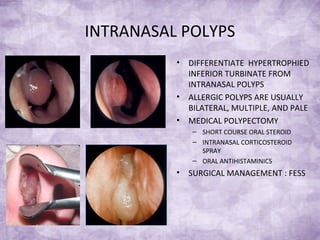
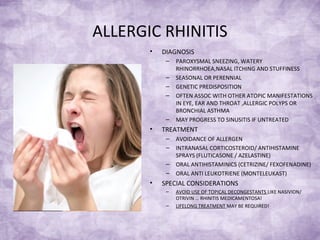
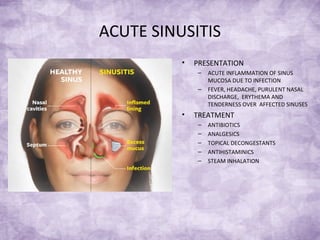
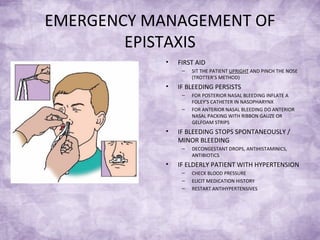
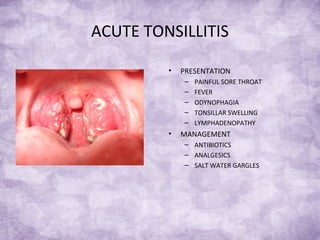
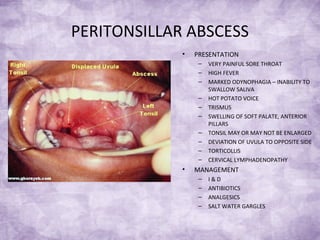
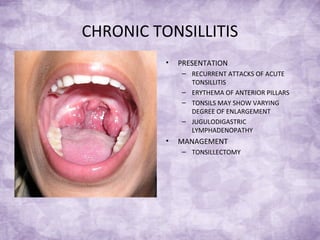
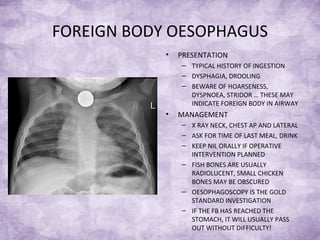
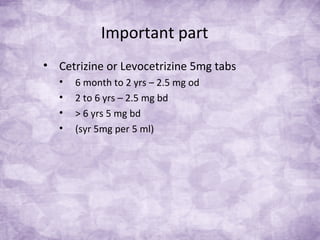
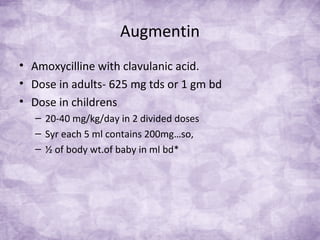
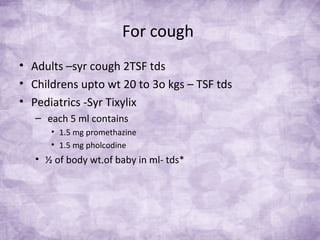
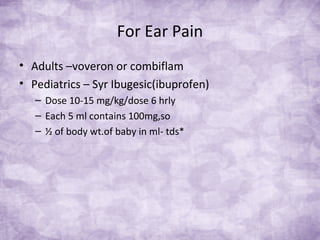
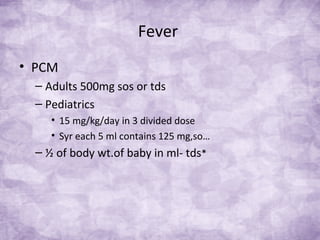
The document provides an overview of common ENT problems, their causes, symptoms, and management strategies. It covers issues related to the ear, nose, and throat, including treatments for various conditions like otitis media, sinusitis, and tonsillitis. Essential management techniques and medications for pediatric and adult patients are also highlighted.